
Author: Vanessa Yu
Mentor: Dr. Andrew Franks
United World College of South East Asia (East Campus)
Abstract
In COVID-19, older adults have been disproportionately vulnerable to illness, death, and psychosocial repercussions. The proposed study aims to explore intersections between the COVID-19 pandemic and ageism among youth. Young adults recruited from the United States will read one of the three passages framing the pandemic in terms of its effects on the U.S. overall, the elderly of the U.S., or the young population of the U.S. and then complete critical measures of COVID-19 attitudes and behaviors. Participant ageist attitude will be included as a moderating variable and perception of the coronavirus as a personal threat will be included as a mediating variable. Conditional process models will be used to examine the direct and indirect effects of risk information on vaccine hesitancy and public health behaviors via the mechanisms of pandemic threat perception across levels of age bias. It is predicted that framing the pandemic in terms of its danger towards young adults will increase reported intentions to adhere to public health guidance via the mechanism of increased perceived threat, particularly for those high in ageism. Potential findings will have strong social, political, and cultural implications for establishing sustainable healthcare systems and intergenerational relationships.
Keywords: ageism, COVID-19, coronavirus, risk perception, public health, information framing
The COVID-19 pandemic has changed nearly all aspects of the daily lives of most individuals, yet those above 65 are disproportionately affected. Through August 2021, older adults have consistently been more prone to pandemic-related illness and death than younger people (Surveillances, V, 2020; Covid et al., 2020); they account for less than 20% of all COVID-19 cases but more than 70% of deaths worldwide (WHO, 2021). Older adults are vulnerable not only to negative physical effects of the coronavirus but also to long-term psychosocial repercussions due to social isolation.
Along with the COVID-19 pandemic, there has been a parallel surge of ageism: from the media’s benevolent portrayal of the older population as a frail, vulnerable group, to hostile discrimination and abuse (Swift et al., 2021). The elderly face detrimental health impacts while having to cope with isolation, loneliness, anxiety, and depression (Banerjee et al., 2020; Bergman et al., 2020). The emergence of ageist attitudes and intergenerational divides have led to critical mental health ramifications on older adults.
Additionally, non-compliance behaviors among adolescents exacerbate the negative impacts on public health. Adolescents are commonly identified with more non-compliance with preventive policies, especially with social distancing, than other age groups (Harris et al., 2021; Nivette et al., 2021; Roy-Chowdhury et al., 2020). Young adults are less likely to display severe COVID-19 symptoms and often consider themselves as immune and invulnerable to the virus (Ayalon et al., 2021; Surveillance, V, 2020). Therefore, as young adults frequently engage in social activities, those infected have high potential of transmitting the virus to others, which ultimately puts the elderly at risk (Andrews et al., 2020). Recently, the Delta variant has become a pressing concern, as infection rate and hospitalization increase dramatically among the younger population (NBC, 2021). Internationally, health officials have been stressing the importance of adhering to health and safety guidelines. However, compliance to recommended health behaviors may be contingent on one’s attitude towards older adults. Accordingly, the current study sought to investigate the conditional indirect effects of reminders of coronavirus risk on adherence to pandemic-related public health behaviors (i.e., vaccine hesitancy, staying home, mask-wearing, physical distancing) as moderated by young adults’ ageism and mediated by perceptions of coronavirus risk.
Participant Ageism
Prior research has demonstrated that ageist attitudes are often strong predictors of adolescent risk-taking behaviors. Young individuals with higher age bias also tend to report higher levels of risk behaviors (e.g., drug use, alcohol use, sexual behaviors) in daily life (Popham, et. al., 2011; Kennison, et. al., 2012). This is consistent with the terror management theory, which suggests that adolescents with strong ageism may attempt to dissociate themselves from their future older selves by seeking experiences that stimulate sensations of youth, strength, and invulnerability (Popham, et. al., 2011). Thus, the present study hypothesizes that youth with higher levels of ageism will also be more likely to engage in risky behaviors and subsequently report lower levels of engagement in COVID-19 protective behaviors. Although little research has been conducted on the specific effects of ageism on COVID-19-related health behaviors in youth, studies indicate that ageist attitudes may be a predictor of behavior change during the pandemic (Vale, 2020).
Risk Information and Risk Perceptions
Risk information indirectly results in attitude and behavior modifications by increasing risk perception and altering emotional responses. Risk information, in the form of novel risk information or reminders of previously-known risks, is positively associated with levels of risk perceptions over time (Gerrard et al., 1999). Numerous studies have found that youth behaviors in risk-taking contexts, such as smoking and sexual behaviors, are responsive to risk information, especially when that information is personally relevant (Dupas, 2011; Gilbert et al., 2017). Moreover, authentic risk perceptions signal the need for preventive measures, and thus influence people’s decision-making and catalyze health behavior modifications in daily life and clinical settings (Edwards, et. al., 2001; Schmälzle, et. al., 2017). Amid past pandemics, such as the MERS outbreak in South Korea and the H1N1 influenza in Britain, increase in the public’s perceived susceptibility to the virus predicted increased preventive behaviors (Bish et al., 2010; Choi et al., 2018). In the COVID-19 pandemic, those perceiving greater risks also tend to report higher compliance with recommended health and safety precautions (de Bruin et al., 2020). Therefore, the present study intends to investigate the link between risk information, risk perceptions, and behaviors in the framework of the coronavirus pandemic.
Research Hypothesis: We hypothesize a conditional indirect effect of exposure to information about the increasing risk of the coronavirus for young adults on COVID-19 health attitudes and behaviors (i.e., vaccine hesitancy, staying home, mask-wearing, physical distancing) that will be moderated by participant ageism and mediated via the mechanism of increased perceptions of personal threat. We predict that exposure to information about the increasing risk of the coronavirus for young adults will cause participants to report increased coronavirus threat perception, which results in reduced vaccine hesitancy and increased health behaviors.
Method
Participants
Participants will be recruited from undergraduate university subject pools from various universities in different areas of the United States. Participants will report their age, gender, race, and political orientation.
Measures
Ageism. Ageism will be measured on the 13-item Ambivalent Ageism Scale (AAS) validated (e.g., Cary et al., 2017) and used (e.g., Vale et al., 2020) by numerous peer-reviewed research studies. An example item is, “It is good to tell old people that they are too old to do certain things; otherwise they might get their feelings hurt when they eventually fail.” Participants will respond to each item on a 7-point Likert scale from 1 – “Strongly Disagree” to 7 – “Strongly Agree,” resulting in a range of possible values on the composite variable from 13 to 91. Higher value indicates greater level of ageism. See Appendix A.
Risk-information. Risk-information will be a manipulated (experimental) independent variable. Participants will be randomly assigned to three condition groups. In each condition, participants will be provided with information that emphasize the continued pandemic-related risks, its widespread impacts, and the importance of vaccination and safety measures. Participants in the threat to older population condition (Condition 2) will read a passage of information emphasizing the continued vulnerability and risks for the older population. Participants in the threat to younger population condition (Condition 3) will read a passage emphasizing the increased vulnerability and risks for the younger population. More details are reported below under “Procedure” and full text is available in Appendix B.
COVID-19 threat perceptions. COVID-19 threat perceptions will be assessed using the 7-item Fear of Coronavirus-19 Scale (FCV-19S) (Ahorsu et al., 2020). The reliability of the scale is validated in different populations (e.g., Perz et al., 2020). An example item is, “I am afraid of losing my life because of coronavirus-19.” Participants will respond to each item on a 5-point Likert scale from 1 – “Strongly Disagree” to 5 – “Strongly Agree,” resulting in a possible range of values from 7 to 35. Higher value indicates greater pandemic-related threat perceptions. See Appendix C.
COVID-19 health attitude and behaviors. Attitudes toward COVID-19 vaccinations will be assessed using three items, “All universities should mandate coronavirus vaccines for all students who are medically able to be vaccinated”, “Employers should mandate vaccinations for all workers who are medically able to be vaccinated, regardless of how otherwise young and healthy those workers are”, and “Everyone who is medically able to receive a vaccine should choose to be vaccinated.” Participants will respond to each item on a 7-point Likert scale from 1 – ”Strongly disagree” to 5 – “Strongly agree.” COVID-19 health compliance behaviors will be evaluated using a 3-items assessing how the framing manipulation has prospectively changed their likelihood to engage in certain behaviors, selected from public health recommendations by the World Health Organization (WHO, 2021), including: (i) stay at home, (ii) adhere to physical distancing (1.5-2m), and (iii) wear a face mask. Participants will indicate on a 7-point Likert scale, from 1 – “I will be much less likely to do this” to 7 – “I will be much more likely to do this,” resulting in a range of values from 3 to 21.
Procedure
Participants will complete an informed consent document and are randomly assigned to read one of the three passages containing information on the number of cases, deaths, and hospitalization among (1) the U.S. population, (2) older adults, and (3) younger adults. All three passages will contain information regarding the rise in cases since the summer of 2021, the threat of the more contagious Delta variant, and the effectiveness of vaccination and preventive behaviors such as social-distancing and mask wearing. Then, participants will report to measures of COVID-19 threat perception, health attitudes, and health behaviors. Finally, participants will complete measures of demographic and personal characteristics (i.e., age, gender, and race) and read a debriefing statement regarding the purpose of the study.
Results
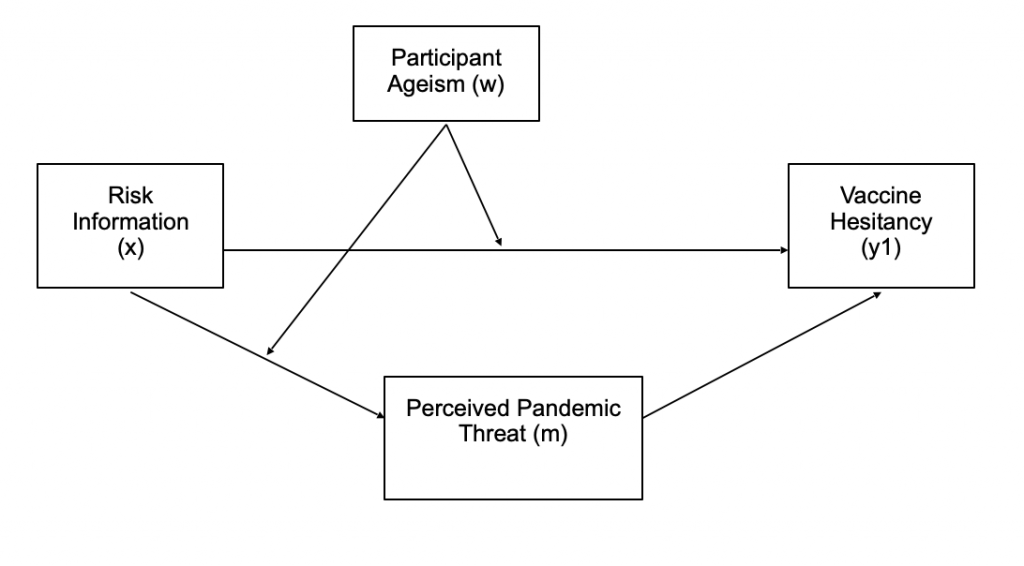
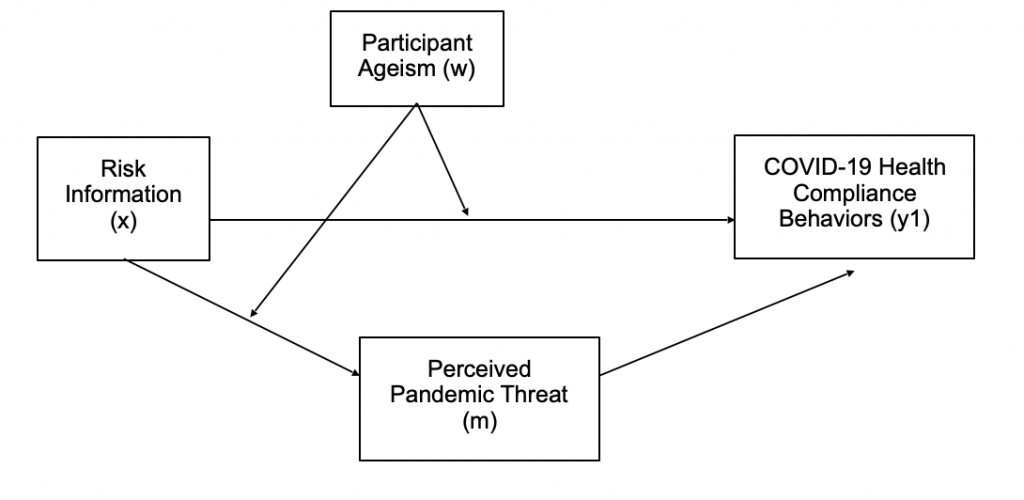
Conditional direct and indirect effects will be examined using PROCESS Model 8 (Hayes, 2013) with risk information as the primary independent variable (x); age-related bias as the moderator (w); perceived coronavirus threat as a mediator (m). Vaccine hesitancy was as the dependent variable (y1) in the first analysis and reported adherence to public health behaviors as the dependent variable (y2) in the second analysis. All indirect effects were computed for each of 10,000 bootstrapped samples and were considered significant if their 95% confidence intervals did not include zero (these bootstrapped effects do not produce exact p values). Non-dichotomous variables were mean centered. The conceptual models are illustrated in Figures 1 and 2.
Discussion
The current study was designed to investigate whether ageism and framing the impact of the coronavirus pandemic in terms of the increased risk of young adults, rather than of the general population or the older population, would predict greater coronavirus threat perception, reduced vaccine hesitancy, and increased health behaviors. We expect that participants with high age bias will report less compliance behaviors and that participants receiving information regarding young adults will also report less compliance behaviors. Overall, we expect to be able to conclude that age bias and framing of risk information have a strong influence on public health outcomes, such as vaccine hesitancy and compliance to safety guidelines.
Implications
The results of this study (if consistent with the hypothesis) will have significant implications for public health and social policy. Ageism in young adults promotes reckless behaviors that jeopardize lives and entire healthcare systems. Reminders of pandemic-related risk that are age-specific and relevant effectively induce attitude modifications and reduce risk behaviors in youth. This accentuates the need for stronger social efforts, including mitigation and information campaigns targeted at young adults (Kolbe, et. al., 1993). In addition, fostering a culture that promotes the value of the lives of older people and reduces the youth obsession that feeds into anti-elderly bias is paramount, especially in a rapidly aging society (Ng & S. H., 1998; North, et. al., 2012; Meisner & B. A., 2021).
Limitations
The study relies on participants’ self-reported response as a measurement of COVID-19 vaccine attitudes and health compliance behaviors. Therefore, the conclusions drawn from this study may be limited by the use of self-reported responses which might not accurately reflect actual behaviors, as participants may be unable or unwilling to report accurate estimates. Additionally, one’s vaccine hesitancy also varies across time, place, and vaccines, yet the assessment of vaccine hesitancy in this study lacks specific vaccine context, thus the results might not generalize to other countries or populations.
Future Directions
The proposed experiment assesses the effects of risk information on COVID-19 health attitudes and behaviors in the short term. Future research may examine whether the observed effects generalize across contexts and to what extent the effects are durable. As research demonstrates that manipulation of information in clinical settings affects patients’ decision-making and health outcomes (Edwards et al., 2001), future research could investigate the effects of framing pandemic-related risk information on public attitudes during the coronavirus pandemic. Future research may also explore the relationship between ageism, risk information, and response (i.e., attitudes and behaviors) in different age groups.
References
Ahorsu, D. K., Lin, C. Y., Imani, V., Saffari, M., Griffiths, M. D., & Pakpour, A. H. (2020). The fear of COVID-19 scale: development and initial validation. International Journal of Mental Health and Addiction, 1-9.
Andrews, J. L., Foulkes, L., & Blakemore, S. J. (2020). Peer influence in adolescence: Public-health implications for COVID-19. Trends in Cognitive Sciences, 24(8), 585-587.
Ayalon, L., Chasteen, A., Diehl, M., Levy, B., Neupert, S. D., Rothermund, K., … & Wahl, H. W. (2020). Aging in times of the COVID-19 pandemic: Avoiding ageism and fostering intergenerational solidarity. The Journals of Gerontology: Series B.
Banerjee, D., D’Cruz, M. M., & Rao, T. S. (2020). Coronavirus disease 2019 and the elderly: Focus on psychosocial well-being, ageism, and abuse prevention–An advocacy review. Journal of Geriatric Mental Health, 7(1), 4.
Bergman, Y. S., Cohen-Fridel, S., Shrira, A., Bodner, E., & Palgi, Y. (2020). COVID-19 health worries and anxiety symptoms among older adults: the moderating role of ageism. International Psychogeriatrics, 32(11), 1371-1375.
Bish, A., & Michie, S. (2010). Demographic and attitudinal determinants of protective behaviours during a pandemic: A review. British Journal of Health Psychology, 15(4), 797-824.
Boehmer, T. K. (2020, October 1). Changing Age Distribution of the COVID-19 Pandemic . . . Centers for Disease Control and Prevention. Retrieved October 6, 2021, from https://www.cdc.gov/mmwr/volumes/69/wr/mm6939e1.htm
Cary, L. A., Chasteen, A. L., & Remedios, J. (2017). The ambivalent ageism scale: Developing and validating a scale to measure benevolent and hostile ageism. The Gerontologist, 57(2), e27-e36.
Choi, D. H., Shin, D. H., Park, K., & Yoo, W. (2018). Exploring risk perception and intention to engage in social and economic activities during the South Korean MERS outbreak. International Journal of Communication, 12, 21.
de Bruin, W. B., & Bennett, D. (2020). Relationships between initial COVID-19 risk perceptions and protective health behaviors: a national survey. American Journal of Preventive Medicine, 59(2), 157-167.
Dupas, P. (2011). Do teenagers respond to HIV risk information? Evidence from a field experiment in Kenya. American Economic Journal: Applied Economics, 3(1), 1-34.
Edwards, A., Elwyn, G., Covey, J., Matthews, E., & Pill, R. (2001). Presenting risk information a review of the effects of framing and other manipulations on patient outcomes. Journal of Health Communication, 6(1), 61-82.
Gerrard, M., Gibbons, F. X., & Reis-Bergan, M. (1999). The effect of risk communication on risk perceptions: the significance of individual differences. JNCI Monographs, 1999(25), 94-100.
Gilbert, H., Sutton, S., Morris, R., Petersen, I., Galton, S., Wu, Q., … & Nazareth, I. (2017). Effectiveness of personalised risk information and taster sessions to increase the uptake of smoking cessation services (Start2quit): a randomised controlled trial. The Lancet, 389(10071), 823-833.
Harris, B., Rigolon, A., & Fernandez, M. (2021). Hiking during the COVID-19 pandemic: Demographic and visitor group factors associated with public health compliance. Journal of Leisure Research, 1-9.
Hayes, A. F., & Preacher, K. J. (2013). Conditional process modeling: Using structural equation modeling to examine contingent causal processes.
Kennison, S. M., & Ponce-Garcia, E. (2012). The role of childhood relationships with older adults in reducing risk-taking by young adults. Journal of Intergenerational Relationships, 10(1), 22-33.
Kolbe, L. J., Kann, L., & Collins, J. L. (1993). Overview of the youth risk behavior surveillance system. Public Health Reports, 108(Suppl 1), 2.
Meisner, B. A. (2021). Are you OK, Boomer? Intensification of ageism and intergenerational tensions on social media amid COVID-19. Leisure Sciences, 43(1-2), 56-61.
NBCNews. (2021, July 15). Minyvonne Burke. Young, unvaccinated people are being hospitalized with Covid-19 as delta variant spreads, officials warn. Retrieved August 20, 2021, from https://www.nbcnews.com/health/health-news/young-unvaccinated-people-are-being-hospitalized-covid-19-delta-variant-n1273998
Nivette, A., Ribeaud, D., Murray, A., Steinhoff, A., Bechtiger, L., Hepp, U., … & Eisner, M. (2021). Non-compliance with COVID-19-related public health measures among young adults in Switzerland: Insights from a longitudinal cohort study. Social Science & Medicine, 268, 113370.
Ng, S. H. (1998). Social psychology in an ageing world: Ageism and intergenerational relations. Asian Journal of Social Psychology, 1(1), 99-116.
North, M. S., & Fiske, S. T. (2012). An inconvenienced youth? Ageism and its potential intergenerational roots. Psychological Bulletin, 138(5), 982.
Perz, C. A., Lang, B. A., & Harrington, R. (2020). Validation of the Fear of COVID-19 Scale in a US College Sample. International Journal of Mental Health and Addiction, 1-11.
Popham, L. E., Kennison, S. M., & Bradley, K. I. (2011). Ageism and risk-taking in young adults: Evidence for a link between death anxiety and ageism. Death Studies, 35(8), 751-763.
Popham, L. E., Kennison, S. M., & Bradley, K. I. (2011). Ageism, sensation-seeking, and risk-taking behavior in young adults. Current Psychology, 30(2), 184-193.
Roy-Chowdhury, V., Perera, D., Tagliaferri, G., Mottershaw, A., & Egan, M. (2020). Young Men Are Hardest to Engage on Coronavirus Guidance: Analysis of 11 Trials with 20,000 UK Adults. Behavioral Insights Team.
Schmälzle, R., Renner, B., & Schupp, H. T. (2017). Health risk perception and risk communication. Policy Insights from the Behavioral and Brain Sciences, 4(2), 163-169
Scobie, H. M. (2021, September 16). Monitoring Incidence of COVID-19 Cases. . . Centers for Disease Control and Prevention. Retrieved October 9, 2021, from https://www.cdc.gov/mmwr/volumes/70/wr/mm7037e1.htm?s_cid=mm7037e1_w
Statista. (2021b, October 8). COVID-19 deaths reported in the U.S. as of October 6, 2021, by age. Retrieved October 9, 2021, from https://www.statista.com/statistics/1191568/reported-deaths-from-covid-by-age-us/
Statista. (2021, October 6). COVID-19 deaths worldwide as of October 6, 2021, by country. Retrieved October 9, 2021, from https://www.statista.com/statistics/1093256/novel-coronavirus-2019ncov-deaths-worldwide-by-country/
Surveillances, V. (2020). The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC Weekly, 2(8), 113-122.
Swift, H. J., & Chasteen, A. L. (2021). Ageism in the time of COVID-19. Group Processes & Intergroup Relations, 24(2), 246-252.
Vale, M. T., Stanley, J. T., Houston, M. L., Villalba, A. A., & Turner, J. R. (2020). Ageism and behavior change during a health pandemic: a preregistered study. Frontiers in Psychology, 11, 3156.
Wark, P. (2021, August 6). Younger adults can get very sick and die from COVID too. Here’s what the data tell us. The Conversation. Retrieved October 10, 2021, from https://theconversation.com/younger-adults-can-get-very-sick-and-die-from-covid-too-heres-what-the-data-tell-us-165250
World Health Organization. (2021, August). WHO COVID-19 Detailed Surveillance Data Dashboard. Retrieved August 16, 2021, from https://app.powerbi.com/view?r=eyJrIjoiYWRiZWVkNWUtNmM0Ni00MDAwLTljYWMtN2EwNTM3YjQzYmRmIiwidCI6Im
Y2MTBjMGI3LWJkMjQtNGIzOS04MTBiLTNkYzI4MGFmYjU5MCIsImMiOjh9
World Health Organization. (2021). Coronavirus disease (COVID-19) advice for the public. 2021. Retrieved August 13, 2021, from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
About the author

Vanessa Yu
Vanessa is an 11th grader at the United World College of South East Asia in Singapore. She is interested in social psychology, mathematics, and physics and also enjoys making and appreciating art.
