Author: Rose Filippazzo
Mentor: Dr. Rosalyn Abbott
Poly Prep Country Day School
Abstract
Elastin, a protein responsible for skin elasticity, undergoes damage during its lifespan from several environmental and internal factors. This causes elastolytic activity and produces elastokines, otherwise known as elastin derived peptides (EDPs), which are responsible for the degradation of elastin. T helper cells, crucial in the adaptive immune response, are impacted by the degradation of elastin. EDPs promote T cell differentiation in favor of Th-1 cytokines, IFN-y, IL-2, and IL-12, by binding to the 67-kDa spliced-galactosidase (S-gal)–elastin receptors (ERC) . The production of Th-2 cytokines counteracts Th-1 cytokines, and vice versa. Therefore, EDPs promotion of Th-1 subsequently suppresses the expression of Th-2 cytokines, IL-4, IL-5, IL-10, and IL-13. Optimal immune scenarios aim to have a balance between Th-1 and Th-2, therefore there is an imbalance favoring Th-1. Elastokines support the development of pathological conditions, which includes but is not limited to, atherosclerosis, emphysema, and chronic obstructive pulmonary disease. In addition, T helper cells are crucial for the immune system by amplifying the immune response, regenerating tissue, and clearing infections. Thus, we investigated the role of elastokines in wound healing and its effects on T-helper cells, specifically Th-1 and Th-2, and hypothesized that EDPs would promote cytokine production and enhance the Th-1 response to release pro-inflammatory signals. Our findings indicated that EDPs result in the polarization of T helper cells in favor of Th-1 cytokine expression, subsequently suppressing Th-2 cytokines. Research indicates EDPs upregulation of Th-1 can contribute to cancer therapeutics. However, excessive upregulation of Th-1 phenotype can cause autoimmune diseases in the central nervous system. Therefore, it is crucial to find a balanced medium between Th-1 and Th-2 expressions.
Keywords: elastin-derived peptides, TH-1, TH-2, adaptive immune system
Introduction
Elastin is a protein consisting of crosslinked tropoelastin polymer molecules bound together in the extracellular matrix of tissue. It is responsible for the elasticity and the resilience of tissues and organs. Elastin is durable and resistant, with a half life of approximately seventy years during which it undergoes little turnover. Throughout this lifespan, it endures damage from the aging process, UV radiation, environmental stressors, enzymic functions, and more. Loss of elastic fiber functions can be caused by enzymic degradation, oxidative stress, binding to proteins or lipids, calcium build up, amino acid racemization, protein modification, and mechanism fatigue. Degradation of elastin also occurs when an organism acquires a wound, which catalyzes the release of proteases. Elastin undergoes further enzymatic degradation when exposed to proteases, particularly elastases, which has the ability to break down elastic fibers. This elastolytic activity causes peptides with biological activity, elastokines, to be released. The effects of elastases and elastokines on elastin cause damage to elastin structures. Elastokines accelerate angiogenesis, upregulate cell activity including cell adhesion, chemotaxis, migration, proliferation, proteases activation, and apoptosis. Elastases combined with elastokines supports the development of pathological conditions, which includes but is not limited to, atherosclerosis, emphysema, and chronic obstructive pulmonary disease (Heinz et al., 2020). Inflammation is the body’s initial, essential response to injury, which is regulated through T helper cells. It has been shown that EDPs activate the 67-kDa spliced-galactosidase (S-gal)–elastin receptors (ERC) , which is associated with cytokine production (Debret et al,. 2005). Thus, we investigated the role of elastokines in wound healing and its effects on T-helper cells, specifically Th-1 and Th-2, and hypothesized that EDPs would promote cytokine production and enhance the Th-1 response to release pro-inflammatory signals. The role of EDPs regulation of Th-2 cells remains unclear. Some evidence indicated it enhances the Th-2 response to combat infectious cells while others have seen a restriction in Th-2 activity.
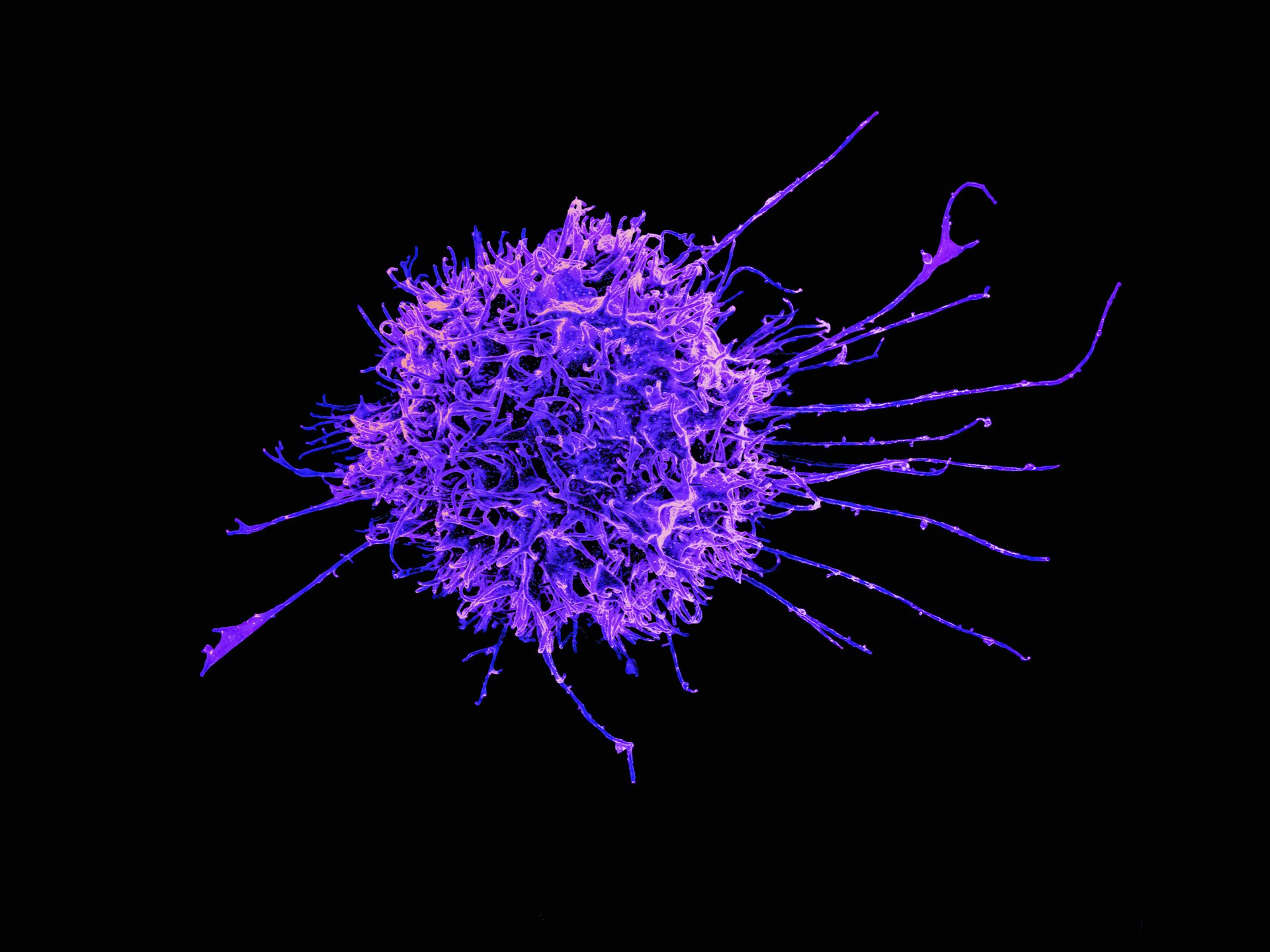
The Immune System: T Helper Cells
The immune system can be characterized into the innate and adaptive system, which work together during wound healing. The innate system is a non-specific, rapid reaction and the body’s first line of defense against foreign bacteria and viruses. The adaptive immune system is a specialized, delayed wound healing reaction that targets specific pathogens not captured by the innate system (NIH, 2006) (Figure 1). One cell type strongly affected by the degradation of elastin is CD4+ T helper cells. T helper cells have five subtypes that each play distinct roles in the immune response, Th-1, Th-2, Th-17, Tfh, and Treg cells. Th-1, which targets cell mediated immunity and protective responses against pathogens, and Th-2, which promotes humoral immunity and released anti inflammatory cytokines, are both part of the immune response that trigger cell remodeling (Romagnani, 2007). Th-1 and Th-2 are produced during cellular immune responses that play a pivotal role in the adaptive immune response. Cytokines are released by the immune system to protect against inflammation when injury occurs, which include Th-1 and Th-2 cells. EDPs cause the activation of cytokine production which subsequently increases T-helper cell subpopulations (Debret et al., 2005). EDPs are a stimulus for Th-1 differentiation, which is crucial for combating pathogens (Figure 2). It also induces a change in the Th-1 phenotype, which causes the secretion of MMP-9, thus promoting tissue remodeling (Maurice et al., 2013). EDPs have been shown to downregulate pro-inflammatory cytokines, such as IL-1, IL-6, IL-8, and TNF-a, in human monocytes, white blood cells crucial for innate immune responses (Maurice et al,. 2013). Although EDPs enhance Th-1 cell response, on stimulation Th-2 cells were reduced (Debret et al,. 2005). Taken together, these signals suggest that EDPs are an important trigger for resolving inflammation and moving into a remodeling phase.
T helper cells are crucial components of the healing process by amplifying the immune response, regenerating tissue, and clearing infections. Without T-helper cells, a host organism would be unable to fight against microbes and the immune system would be severely compromised (Alberts et al., 2002). Elastokines are typically considered detrimental because they occur during the degradation of elastin. Less is known about their beneficial effects, such as their signalling ability in immune cell migration. Little research has been conducted on the interplay and communication between elastokines and other elastin receptors (Heinz et al., 2020).
EDPs effect on Th-1
EDPs are a crucial regulator for Th-1 activation. When testing the effects of EDPs on human peripheral blood lymphocytes (PBLs), researchers exposed T cells to EDPs under different conditions. This included activated, non activated, and cytokine induced T cells. Th-1 and Th-2 cytokine production was quantified to demonstrate which T helper cell was more prevalent. They concluded that EDPs shifted T helper cells to Th-1 cytokine production (IL-2, IFN-y, IL-12), therefore enhancing the Th-1 phenotype (Debret et al., 2005) (Figure 2). Th-1 cytokines are responsible for the proinflammatory responses to eliminate intracellular parasites and enhance autoimmune responses (Berger, 2000). Therefore, EDP triggered upregulation of Th-1 cells is likely an adaptive immune response indicating cellular immunity against pathogens and other viruses.
EDPs effect on Th-2
Although EDPs do not directly suppress Th-2, it occurs consequently through the enhancement of Th-1. A surplus amount of proinflammatory cells can cause tissue damage, thus revealing the necessity to mediate Th-1 overproduction. Th-2 cytokines, IL-4, IL-5, and IL-13, produce IgE, a type of antibody. IgE has been shown to counteract IL-12, which is produced by Th-1 cytokines, and skews T cell differentiation in favor of Th-2 production. Th-2 cytokines also cause the activation of eosinophilic which inhibits Th-1 activation. Th-2 cytokines also include IL-10, which has an anti-inflammatory response. The production of Th-2 cytokines therefore counteracts Th-1 cytokines, and vice versa. Therefore, since EDPs enhance Th-1, they subsequently inhibit Th-2. Optimal immune scenarios aim to have a balance between Th-1 and Th-2. Previous studies indicate Th-2 can be reduced through increased allergen dosage, mycobacterial vaccines, and pregnancy or early postnatal life (Berger, 2000).
Medical Use of T helper Cell Regulation
EDPs upregulation of Th-1 could be beneficial in combating cancer. Upregulation of Th-1 response has demonstrated beneficial in curing tumors. In experimental mice with cancer, those with recurring tumors experienced decreased levels of CD44+3CD621- effector memory T cells. Therefore, tumor relapse was associated with a return to Th-2 microenvironment. Mice who remained regressed were observed to have increased Th-1 genes (Tbx21, IL12, IFNγ, and TNFα) and low Th-2 genes (Gata3, IL4, TIM3) (Dai et al., 2018).
Excessive upregulation of Th-1, known as Th-1 dominance, can worsen organ specific autoimmunity. Overexpression of the Th-1 phenotype can cause autoimmune diseases in the central nervous system. Excess production of IFN-y has the potential to produce inflammatory lesions and excess IL-12 can accelerate collagen induced arthritis. Current therapeutics to mediate Th-1 dominance include TNF-α inhibitors , corticosteroids, and immunosuppressants. In a study conducted on mice, a lack of Th-1 and upregulation of Th-2 protected the development of T-bet diseases, a transcription factor crucial for immune responses (Dardalhon et al., 2008). Th-2 dominance can be caused by allergic and autoimmune diseases. Therapeutics to combat overexpression of Th-2 include Th-2 cytokine antibodies and mast cell stabilizers.
Conclusion
T helper cells’ response is crucial for understanding the immune system. Elastokines, a typically negative bodily response to the degradation of elastin, have exhibited beneficial effects in enhancing Th-1 cytokines and restricting Th-2 cytokines to produce a balanced immune response. This is achieved by binding to the ERC which triggers an inflammatory response and differentiation of T cells to the Th-1 phenotype. Th-1 cytokines then suppress the over-expression of Th-2 cytokines, which fight against larger pathogens, but over-expression can cause allergic diseases. EDPs interact with T helper cells to promote Th-1 differentiation. The enhancement of Th-1 and cytokines it produces directly counteracts the expression of Th-2 cytokines. While elastokines have been suggested as an approach for treating osteoarthritis, excessive upregulation of Th-1 can cause detrimental long term effects, causing the necessity to find a mediated amount of Th-1 regulation. Since elastokines’ role is to upregulate tissue damage and inflammation, using them to treat T helper cells is typically not a favorable approach (Debret et al., 2005). Therefore, more research is necessary to not only focus on upregulation of Th-1, but to find a balanced medium. Overall, less is known about the adaptive immune system. This research provides insight into the proinflammatory responses which occur in the system and can be beneficial for improving or dictating new wound healing therapeutics.
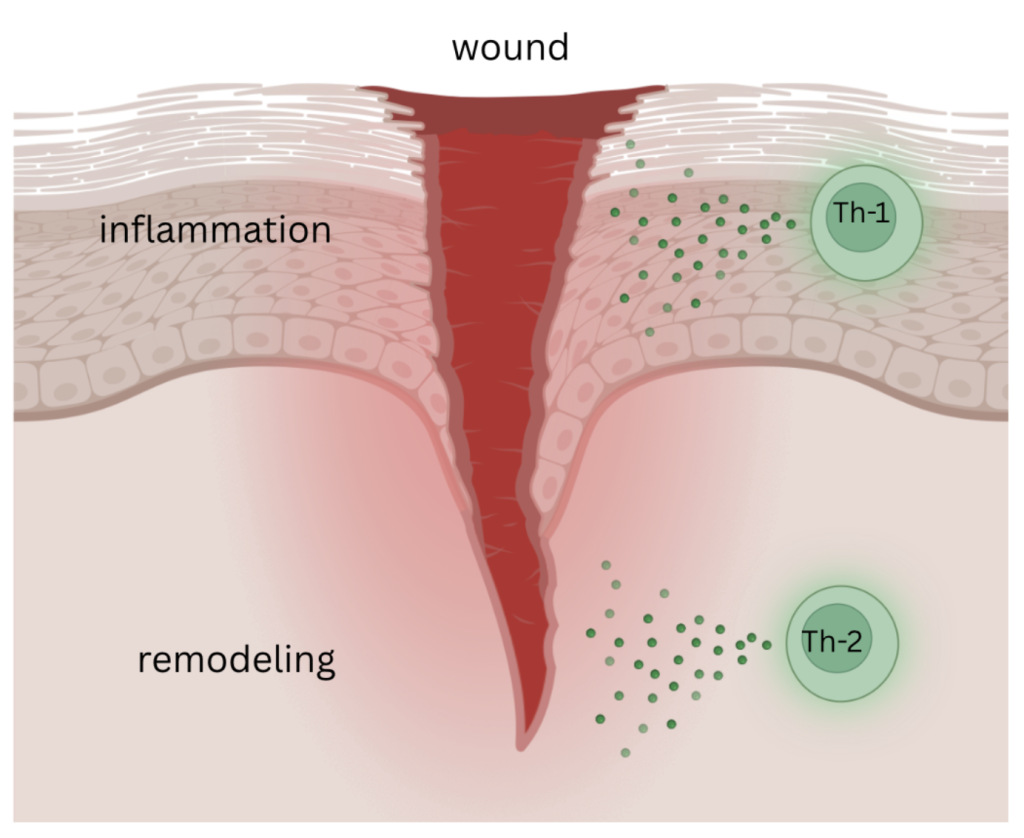
Figure 1. Wound environment with upregulation Th-1. Th-1 comes first in the healing process and releases cytokines (IFN-y, IL-2, and IL-12) responsible for inflammation. Then Th-2 releases cytokines (IL-4, IL-5, IL-10, and IL-13) necessary for remodeling and tissue construction.
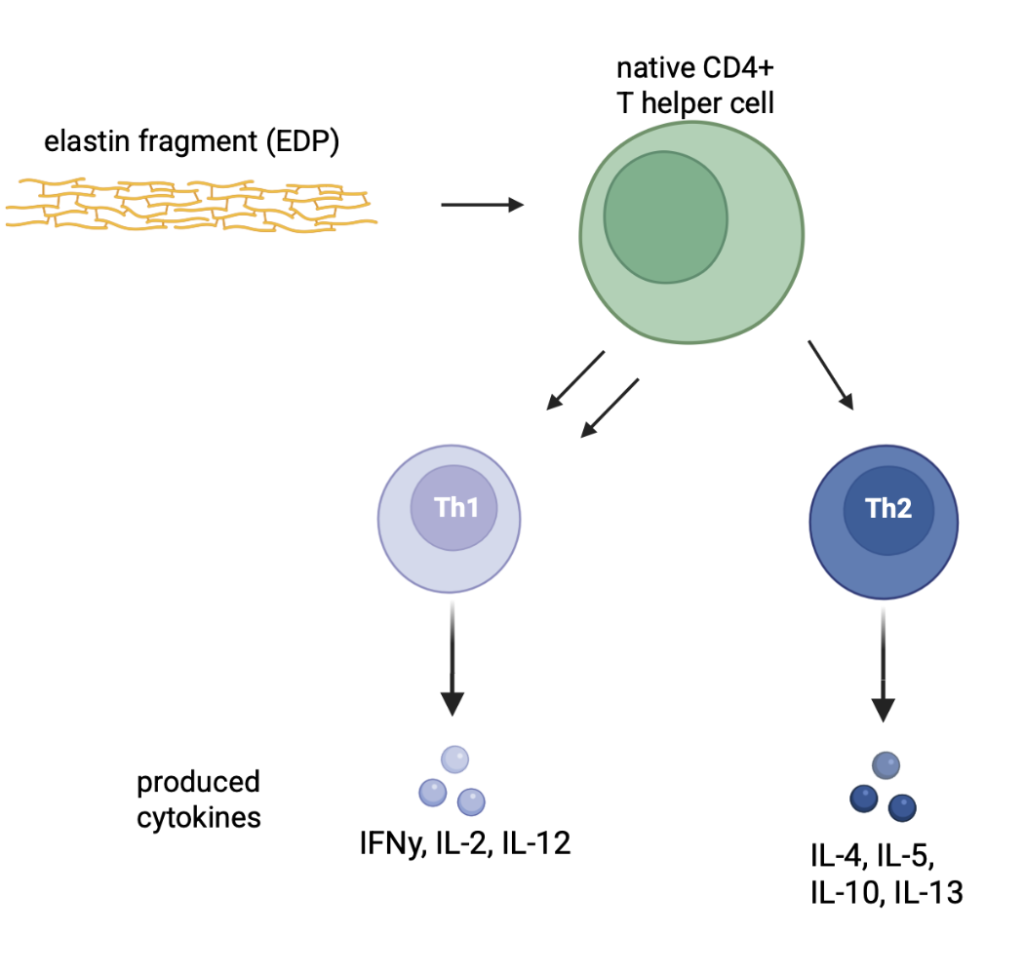
Figure 2: Elastin fragments attach to the ERC located on the native CD4+ T helper cell. This interaction promotes Th-1 cell differentiation, causing more Th-1 to be produced than Th-2. The cytokines from Th-1 are IFN-y, IL-2, and IL-12 The cytokines produced from Th-2 are IL-4, IL-5, IL-10, and IL-13.
References
Full article: Elastases and elastokines: Elastin degradation and its significance in health and disease . (n.d.). Retrieved September 14, 2025, from https://www.tandfonline.com/doi/full/10.1080/10409238.2020.1768208
Berger, A. (2000). Th1 and Th2 responses: What are they? BMJ (Clinical Research Ed.) , 321 (7258), 424. https://doi.org/10.1136/bmj.321.7258.424
Elastin-Derived Peptides Induce a T-Helper Type 1 Polarization of Human Blood Lymphocytes | Arteriosclerosis, Thrombosis, and Vascular Biology . (n.d.). Retrieved September 14, 2025, from https://www.ahajournals.org/doi/10.1161/01.ATV.0000168412.50855.9f
Elastin fragmentation and atherosclerosis progression: The elastokineconcept—ScienceDirect . (n.d.). Retrieved September 14, 2025, from https://www.sciencedirect.com/science/article/abs/pii/S1050173812004616?via%3Dihub
Th1/Th2 Cells | Inflammatory Bowel Diseases | Oxford Academic . (n.d.). Retrieved September 14, 2025, from https://academic.oup.com/ibdjournal/article-abstract/5/4/285/4753946?redirectedFrom=fulltext
Dai, M., Hellstrom, I., Yip, Y. Y., Sjögren, H. O., & Hellstrom, K. E. (2018). Tumor Regression and Cure Depends on Sustained Th1 Responses. Journal of Immunotherapy , 41 (8), 369–378. https://doi.org/10.1097/CJI.0000000000000231
Role of Th1 and Th17 cells in organ-specific autoimmunity—ScienceDirect . (n.d.). Retrieved September 14, 2025, from https://www.sciencedirect.com/science/article/abs/pii/S0896841108000504?via%3Dihub
Romagnani, S. (2008). Human Th17 cells. Arthritis Research & Therapy , 10 (2), 206. https://doi.org/10.1186/ar2392
In brief: The innate and adaptive immune systems—InformedHealth.org—NCBI Bookshelf . (n.d.). Retrieved September 14, 2025, from https://www.ncbi.nlm.nih.gov/books/NBK279396/
B, A., A, J., & J, L. (2002). Molecular Biology of the Cell (4th edition). Garland Science. https://www.ncbi.nlm.nih.gov/books/NBK26827/
About the author

Rose Filippazzo
Rose is a junior currently living in Brooklyn, New York. She enjoys taking Science Research classes through her school and is interested in pursuing a career in medicine. Outside of academics, Rose enjoys playing volleyball and helps lead several service endeavors, which include refurbishing and donating assistive technology to public schools and fundraising through the Anthony Filippazzo Grant for Williams Syndrome Research.