Author: Ankith Sureddi
Mentor: Dr. Hong Pan
Alexander W. Dreyfoos School of the Arts
Abstract
One of the most significant public health crises in the United States is the opioid epidemic. The opioid epidemic is categorized by misuse of opioids such as heroin, prescription opioids, and synthetic opioids such as fentanyl. The rise in the use of opioids has led to increased overdoses due to the increase in accessibility to this class of drugs. The increase in the opioid epidemic is not only due to how accessible opioids are but also how addictive they are due to how they increase feelings of euphoria in the brain.
| Terms: | Definitions: |
| Opioid Substance Use Disorder | The chronic use of opioids causes significant impairment with symptoms such as increased withdrawals and desire to use such substances. |
| Social Determinants of Health | Nonmedical factors which influence health outcomes such as an individual’s age, work, lifestyle, etc. These factors are largely shaped by economic policies and social norms along with political systems. |
| Opioids | Pain relievers available legally for prescription when it comes to pain management are highly addictive and have been involved in the majority of overdose deaths in the U.S. |
| Cellular Receptors/receptors | Proteins located internally or externally of a cell receive a signal to be able to communicate to itself or other cells. What binds to the receptor to create a chemical signal is a ligand, which is the chemical messenger. |
| Public Health | The area of study and field focuses on the improvement of health in the population through education on disease prevention, substance abuse, and environmental health. |
| Epidemic | Widespread infectious disease in a community at a specific period. |
Introduction (The Origins and Escalation of the Opioid Epidemic):
United States Overdose Deaths:
Box 1: Waves of the Opioid Epidemic
- Prescription Opioids: Classes of drugs physicians or healthcare workers prescribe to patients to relieve pain in the body.
- Overdose deaths: When an individual takes a drug more than the quantity needed, which can often lead to death or other harmful complications.
- Heroin: An opioid drug that consists of morphine
- Synthetic opioids: Opioids that are made in laboratory settings and act similarly or the same in the brain as natural opioids to reduce pain (increasing pain tolerance).
My Interest
One day while I was shadowing in the ER with a doctor, we went into one of the ER rooms where I saw a homeless man who was not feeling well. He could barely speak. He did not answer any of the doctor’s or nurses’ questions. However, the only words he used in his voice were to utter “I just want some opioids.” I was shocked that he did not care about his health and all he cared about were opioids. At the time I did not understand what opioids were but then when I learned more about them from the ER doctor and how addictive they can be, I realized that opioid addiction is an epidemic in the United States. Substances such as opioids are often used by individuals as a coping mechanism to manage pain and relieve symptoms of serious illnesses but many also get addicted in the process.
Background
Because substances such as opioids alter the mental and physical state of a person, these substances have a higher potential for misuse. Misuse can be when individuals use the substance more than the recommended prescription dose to produce the desired mind-altering effect. Even though the desirable effect may be achieved by using the substance in accurate doses, misuse can cause negative consequences both physically and mentally. Substance abuse is commonly categorized as a mental health disorder. Individuals who have health complications fail to meet dosing guidelines as prescribed and take higher doses which leads to dependence and addiction. One substance that has been commonly abused is prescription opioids (Opioids, 2024).
Opiates are a class of painkillers that come either directly from the opium poppy or manufactured in a laboratory and are one of the oldest pain-relief drugs. Common opiates are codeine, heroin, morphine, and fentanyl with the most common opiates being prescription opioids and heroin (Bolshokova et al., 2019). Opiates are effective analgesics, a medication that treats pain and inflammation (Wang et al, Wang).
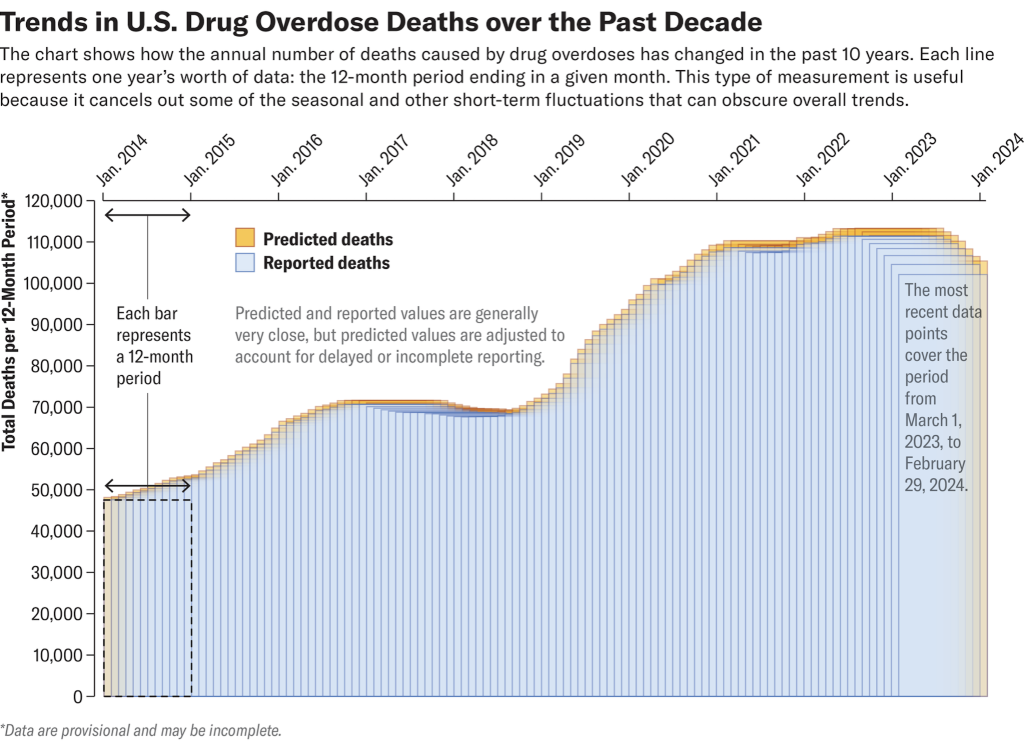
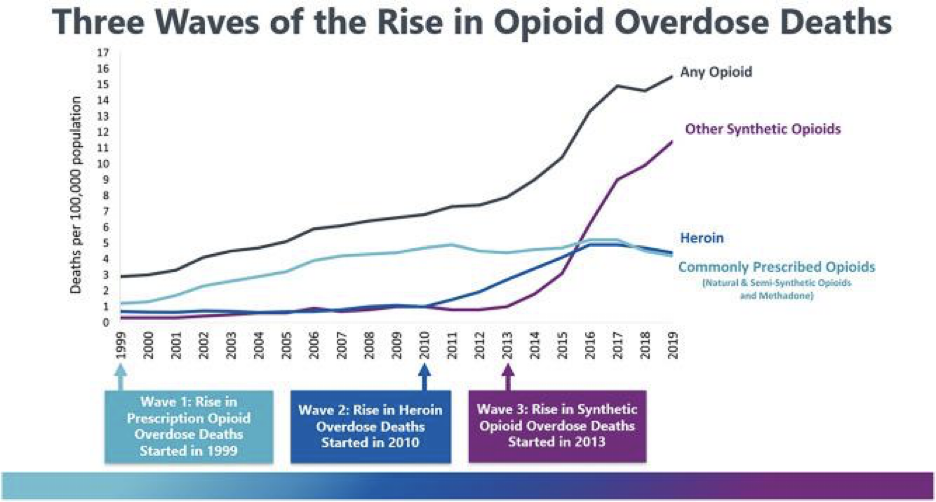
Common opiates are heroin, morphine, and fentanyl with the most common opiates being prescription opioids and heroin (Bolshokova et al., 2019). There have been three waves when it comes to the rise in opioid overdose deaths during the opioid epidemic: a rise in prescription opioid overdoses, heroin overdoses, and synthetic opioid overdoses. Heroin and prescribed opioid overdoses are slowing down due to abuse-deterrent formulations, overdose deaths have also recently lowered from 2023 to 2024 due to the betterment of the pandemic, and synthetic opioid overdoses are increasing at a fast rate. The opioid epidemic is still very much prevalent and needs to be mitigated even more (Lewis, 2024).
This paper will present why opioids are highly addictive by discussing the molecular aspect of opioids and how opioids interact with the brain, the intersection between social determinants of health and the opioid epidemic, who is most impacted, and public health initiatives and solutions that need to be taken to mitigate the opioid epidemic.
How Opioids Hijack the Brain and Cause Negative Side Effects:
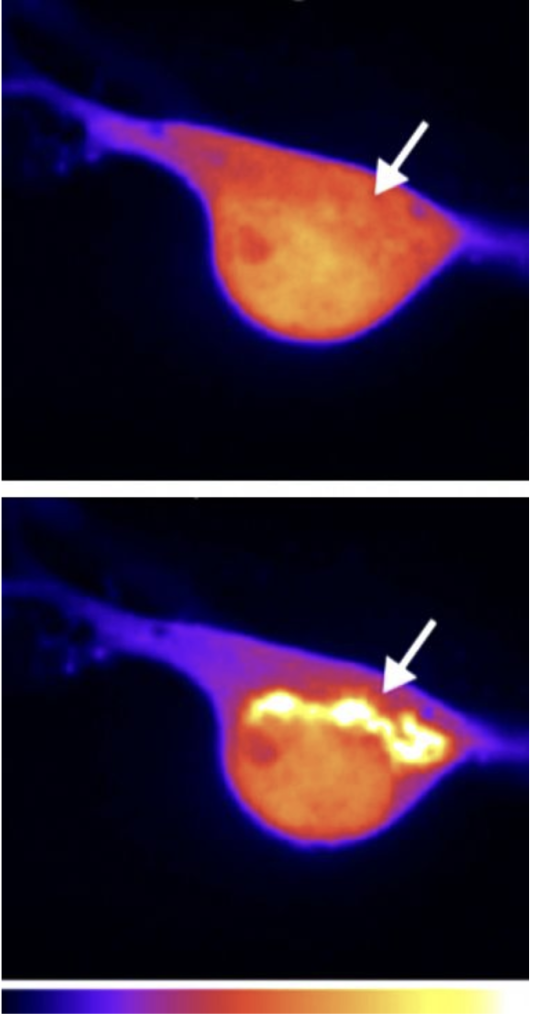
Disinhibition of GABA:
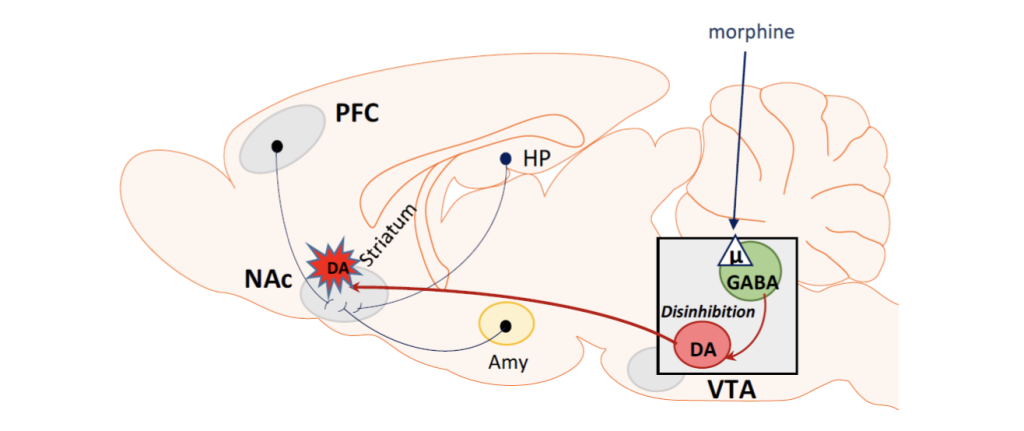
Figure 3 – This figure illustrates the effects of morphine (a type of opioid drug) on the brain. Morphine interacts with the brain to create a rewarding feeling for the individual by impacting the chemical GABA (which is responsible for the release of dopamine). Morphine inhibits the reduction of the release of dopamine (A neurotransmitter or hormone in the brain that creates feelings of pleasure in individuals) by GABA and instead allows increased release of dopamine. By releasing the increased amounts of dopamine in the brain, opioids such as morphine become highly addictive as a result (Listos, 2019).
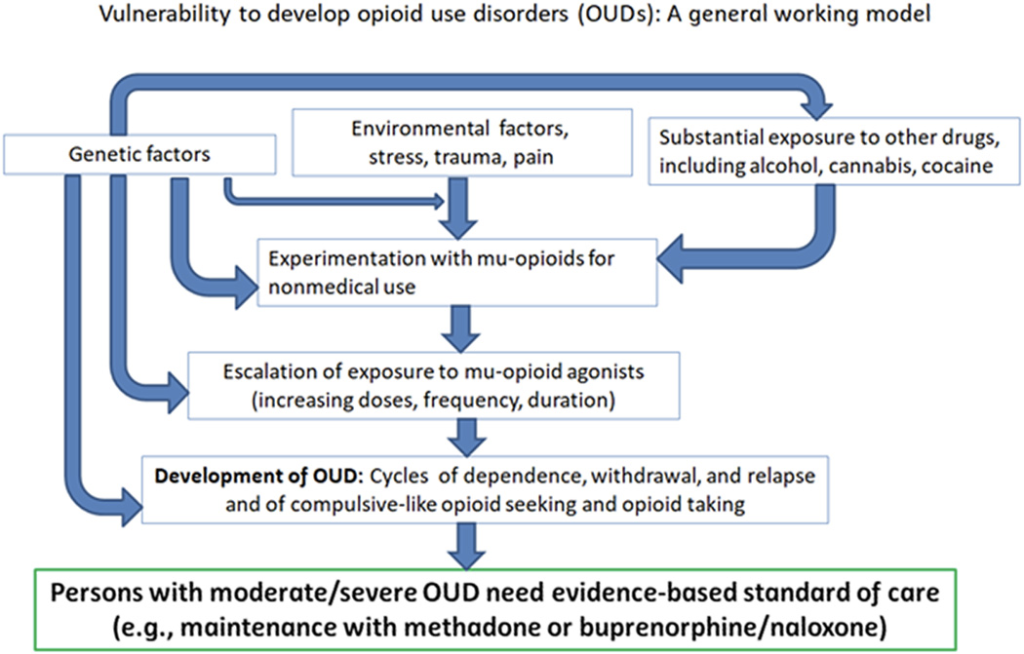
How Vulnerability in Opioid Use Disorders Occur:
Activation of Opioid Receptor by Opioid:
The Molecular Impacts of Opioids and Their Side Effects:
- Nerve Cells: Types of cells in the body that send messages from the body to the brain or the other way around.
- Opioid Receptor Activation: Opioids bind to the opioid receptor, causing activation to occur where the pain relief begins to occur.
Molecular Aspect of Opioids
Opioids function by activating the opioid receptors on the nerve cells. Opioids act as ligand molecules (molecules that attach or bind to other molecules) and attach to the opioid receptors (Proteins that act as communication between the internal cellular membrane and the external environment by interacting with and binding to either drugs or neutron emitters. These receptors are found on the surface of the cell membrane) in the body such as in the spinal cord, brain, etc. When opioids bind to the opioid receptors in the body, they inhibit pain messages through the spinal cord to the brain (How Opioid Drugs Activate Receptors, 2018).
While blocking pain, these opioids can also increase euphoric feelings and emotions by activating the reward pathway in the brain. Opioids have a high potential for misuse and addiction due to the euphoric response and addictive properties as well as causing respiratory depression, which all contribute to the ongoing opioid crisis (Bolshokova et al., 2019). Opioid receptors are often involved in various physiological functions and side effects such as pain modulation, euphoria, sedation, cardioprotection, neuroprotection, and respiratory depression (Shenoy et. al, 2023).
Side Effects
Some of the less common types of side effects from opioid addictions are delayed gastric emptying, muscle rigidity, immunologic and hormonal dysfunction, cardiac arrhythmia, pruritus, xerostomia, and hyperplasia (Koptnik et. al, 2023). Opioid addicts may not fully comprehend the extent of their impairment from the opioids, causing them to attempt to operate machinery that could cause them to be dangerous to themselves and others such as driving a car while under the influence of opioids. While chronic opioid users may not have impairments such as those taking it for the first time because of their tolerance to the drug, long-term opioid use can lead to other neurocognitive deficits (Opioid Use Disorder, 2021).
Uncovering the Faces Who Are Impacted Most by the Opioid Epidemic:
Box 3: The Intersection between Social Determinants and the Opioid Epidemic
Determinants concerning Opioid Use:
Risk Factors Leading to Opioid Use:
The Impacts of Social Determinants on the Opioid Epidemic:
- Neuropsychiatric: Medical field combining psychiatry and neurobiology to see how behavior is impacted.
- Allelic variations: Number of various alleles that form at specific parts on a chromosome.
- Chromosome: Located in the nucleus of a cell, structures that are composed of DNA.
- SUD (Substance Use Disorder): a disorder that leads to negative health harms due to the inability to control substance addiction.
- Social Position: An individual’s social class in life.
- Family System Challenges occurring in the family unit related to emotional, life transitions, etc.
Who is impacted by the Opioid Epidemic
There has been a recent rise in opioid addictions especially in urban settings. This is mainly due to the easy accessibility of fentanyl-contaminated heroin on the streets which is highly addictive and in some cases deadly. Fentanyl is a type of synthetic opioid that has been known to be mixed with illicit drugs to make it easier for users to have a high. Often because of the lethal doses of fentanyl mixed with other drugs, it has caused a large increase in overdoses (What if Fentanyl, 2021).
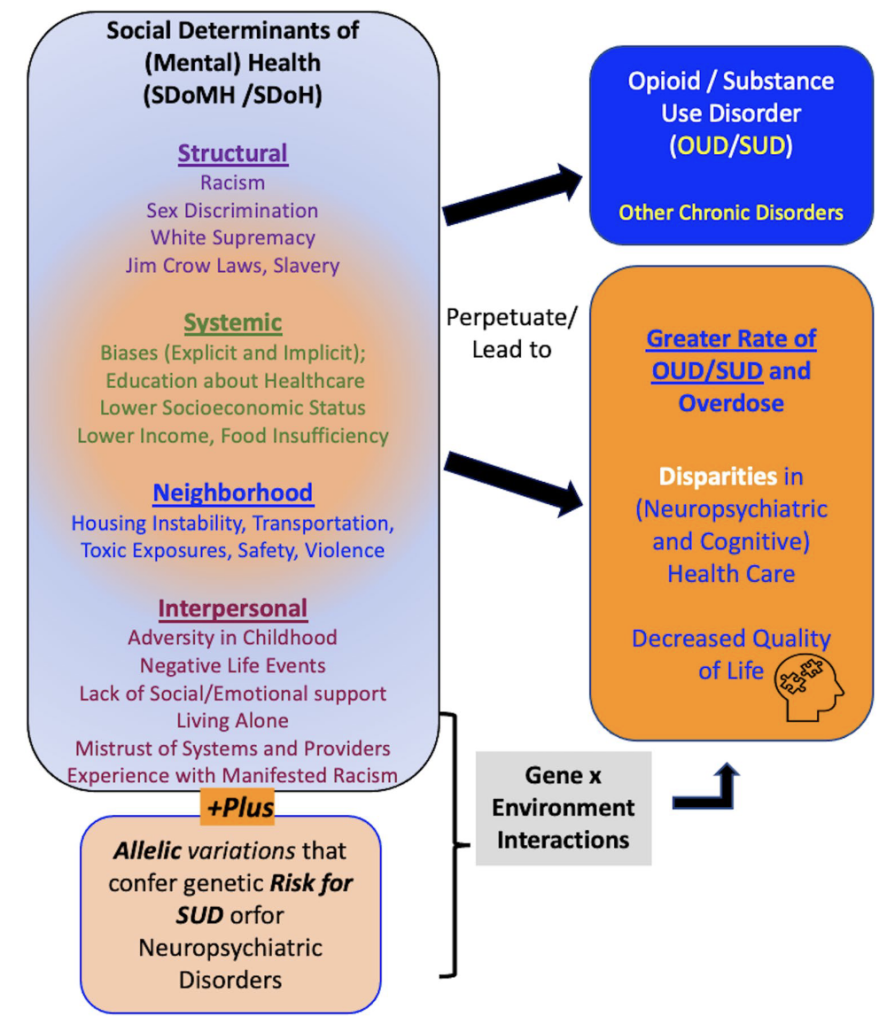
This epidemic has especially impacted the African American population in the U.S. during and after the COVID-19 pandemic. This can be due to the biased prescribing of opioids. There has been a huge increase in the prescription of opioids to certain populations in society based on race and ethnicity. Whites are being prescribed opioids for emergencies while more Blacks are prescribed for surgical intervention or cancer treatments. This has been associated with increased social stigma and mental health disorders combined with greater genetic risk which has led to an increase in the illicit use of opioids and painkillers leading to an increase in the epidemic and an increase in overdose deaths in certain races and ethnicity populations (Gondré-Lewis et. al, 2022).
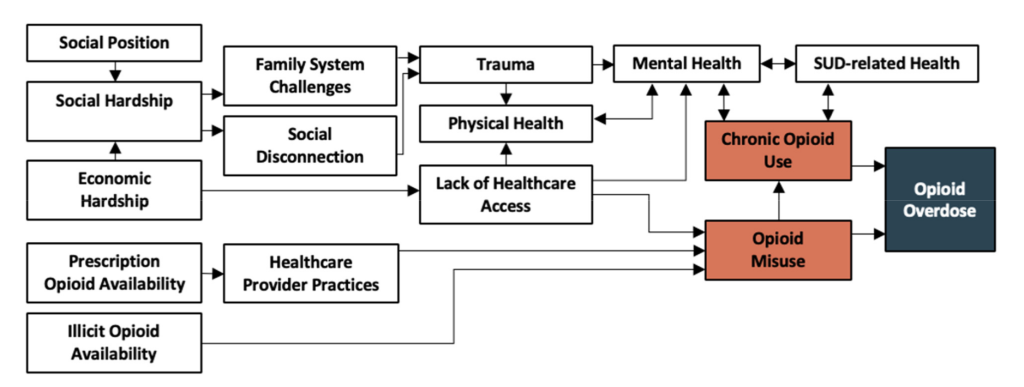
Social Determinants Intersection with the Opioid Epidemic
Social determinants of health play a key role in specific populations such as minorities and poorer populations in becoming more addicted to and exposed to opioids than their white counterparts. Types of social determinants are systemic, structural, neighborhood, and interpersonal. Especially in populations and communities with a lack of access to proper healthcare or healthcare at all, opioid misuse and overdose have been exacerbated. However, this can also go the other way where individuals with greater access to prescription opioids with more access to healthcare systems have also a great chance of opioid misuse and overdose. Individuals who are full-time employees, have private insurance, are of older ages, and have higher education levels have had the most success in completing treatment against opioid use. Surprisingly, patients from the criminal justice system who were sent for treatment also had high rates of treatment completion. However, the success of treatment completion and increased rates of treatment completion decreased with each previous additional attempt at treatment (Gondré-Lewis et al., 2022).
When researching completion and rehabilitation treatment programs that were funded publicly in the United States, it was found that opioid-use patients completed treatment in states with greater availability of treatment facilities that accept state insurance and adjusting prices based on the ability and means of the patient to be able to pay for treatment. Individuals in states with a large amount of population living in rural regions mostly had lower completion rates for treatment while residential treatment (Patient care in a non-hospital setting focusing on treating mental health and substance abuse issues in patients) patients had greater success (about four times greater success) in treatment completion rates. It was also found that patients who have longer wait times for treatment were less likely to follow up on their treatment and complete it compared to those who had to barely wait or even had to wait zero days (Kreek, 2019).
The Vital Role of Legislation and Public Health in Creating a Healthier Future:
Solutions in the Healthcare Setting
To be able to limit the opioid epidemic, healthcare providers need to play a major role in mitigating this epidemic. Healthcare providers can limit opioid prescriptions, encourage patients to participate in exercise therapy, alternate treatment options (such as NSAIDs, serotonin-norepinephrine re-uptake inhibitors, tricyclic antidepressants, etc.), guide patient education in risks of addiction, monitor drug monitoring programs, and work with teams such as therapists and pharmacists to understand a patient’s medication history to optimize medication safety (Koptinik et. al, 2023).
One of the largest causes of the opioid epidemic is individuals getting opioids from patients who are their family or friends in an attempt to self-medicate for pain. The Mainstreaming Addiction Treatment (MAT) Act provision expands evidence-based therapies by expanding the availability of evidence to mitigate the opioid epidemic. This act allows healthcare workers to have a controlled standard when it comes to prescribing buprenorphine for opioid use disorder (OUD) to integrate substance use disorder treatment in various healthcare settings (Dydyk et. al, 2024). Universal prevention, which emphasizes drug usage fear and increasing education on the negative impacts of drug usage, is very effective in decreasing drug usage rates. Regulatory prevention has also been found to decrease drug availability via laws or taxes and has been lowering levels of harm for younger populations when it comes to accessible substances but can be hard to do when it comes to prescription-based drugs only obtained from medical professionals. Instead, addicts receive prescription opioids from family or friends who have been prescribed opioids for pain management purposes (Edemekong, et. al).
The CDC recommends only prescribing opioids when deemed necessary and usage be carefully monitored by a healthcare professional and that non-opioid therapy should be instead used for pain management unless extreme cases such as when a patient is battling cancer or undergoing end-of-life care with the main goal of preventing abusing prescription opioids. Some examples of replacements for opioids include tricyclic antidepressants, topical agents, muscle relaxants, and nonsteroidal anti-inflammatory drugs. When it comes to treatment plans, healthcare workers should provide treatment goals and expectations to patients whenever prescribing opioids to patients is necessary with 1-4 weeks follow-up being best to evaluate progress and monitoring for every three months to determine if opioid use is required. The CDC states that three days of pills or less are needed and seven days is only for rare cases when it comes to pain relief. Before prescribing patients opioids, it is recommended that doctors assess a patient’s substance abuse and depression history (as they may act as risk factors for substance abuse) (Guideline Recommendations and Guiding Principles, 2022).
Legislation Efforts
In terms of legislation, a prescription drug monitoring program (PDMP) has been implemented by the United States. This program allows healthcare workers to verify if prescribed opioids were given to patients from other medical sources in a state-based database system, which has been found to significantly reduce “doctor shopping” (opioid addicts going to multiple medical sources and healthcare workers to be prescribed opioids). The issue with the PDMP is that these programs are not utilized as much by medical professionals and take a long time to retrieve information on opioid prescriptions. Oregon established a statewide coalition named the Oregon Coalition for Responsible Use of Medications (OrCRM) to reduce overdoses and misuse of medications such as opioids through community engagement with a community effort to mitigate opioid-related overdoses. This has been done by partnering with members of the community in businesses such as law enforcement, healthcare, churches, and public health offices. This strategy has been proven to be effective (Holton et. al, 2018).
Conclusion
The opioid epidemic is a type of crisis that is impacted by various factors such as health disparities, risk factors, etc. Opioids are used for pain management but are highly addictive drugs because opioids impact the release of dopamine by inhibiting GABA, causing increased dopamine levels. To better the opioid epidemic and mitigate its impacts, there needs to be an effort between everyone in the community by working with healthcare workers and institutions, education institutions, and government institutions. Public policy is important when it comes to mitigating the opioid epidemic by implementing more policies regarding opioid monitoring programs to prevent the overprescribing of opioids. More policies on increasing access to opioid addiction treatment centers and increasing education on opioid addiction should also be done to combat the opioid epidemic. Especially focusing on the at-risk populations such as those of poorer communities or minority communities, would be a large step toward mitigating the opioid epidemic and its impact on society. Ultimately, the opioid epidemic needs to be combated and this can only be done by focusing on effective public health initiatives and taking multifaceted approaches by working with not only healthcare institutions but also public policy and educational institutions.
Acknowledgments:
The author would like to acknowledge Dr. Pan for his support and guidance during the research and publishing of this paper.
Work Cited:
Abuse, N. I. on D. (2021a, June 1). Fentanyl DrugFacts | National Institute on Drug Abuse (NIDA). https://nida.nih.gov/publications/drugfacts/fentanyl
Abuse, N. I. on D. (2021b, June 1). Prescription Opioids DrugFacts | National Institute on Drug Abuse (NIDA). https://nida.nih.gov/publications/drugfacts/prescription-opioids
Abuse, N. I. on D. (–). Opioids | National Institute on Drug Abuse (NIDA). https://nida.nih.gov/research-topics/opioids
Bolshakova, M., Bluthenthal, R., & Sussman, S. (2019). Opioid use and misuse: Health impact, prevalence, correlates and interventions. Psychology & Health, 34(9), 1105–1139. https://doi.org/10.1080/08870446.2019.1622013
Brady, B. R., Taj, E. A., Cameron, E., Yoder, A. M., & De La Rosa, J. S. (2023). A Diagram of the Social-Ecological Conditions of Opioid Misuse and Overdose. International Journal of Environmental Research and Public Health, 20(20), 6950. https://doi.org/10.3390/ijerph20206950
CDC. (2024a, May 6). Guideline Recommendations and Guiding Principles. Overdose Prevention. https://www.cdc.gov/overdose-prevention/hcp/clinical-guidance/recommendations-and-principles.html
CDC. (2024b, September 10). Social Determinants of Health (SDOH). About CDC. https://www.cdc.gov/about/priorities/why-is-addressing-sdoh-important.html
Definition of nerve cell—NCI Dictionary of Cancer Terms—NCI (nciglobal,ncienterprise). (2011b, February 2). [nciAppModulePage]. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/nerve-cell
Dydyk, A. M., Jain, N. K., & Gupta, M. (2024). Opioid Use Disorder. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK553166/
Edemekong, P. F., & Tenny, S. (2024). Public Health. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK470250/
Holton, D., White, E., & McCarty, D. (2018). Public Health Policy Strategies to Address the Opioid Epidemic. Clinical Pharmacology and Therapeutics, 103(6), 959–962. https://doi.org/10.1002/cpt.992
How opioid drugs activate receptors. (2018, May 21). National Institutes of Health (NIH). https://www.nih.gov/news-events/nih-research-matters/how-opioid-drugs-activate-receptors
Kopitnik, N. L., & Huecker, M. R. (2024). Opioid Prescribing. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK551720/
Kreek, M., Reed, B., & Butelman, E. (2019). Current status of opioid addiction treatment and related preclinical research. Science Advances, 5, eaax9140. https://doi.org/10.1126/sciadv.aax9140
Lewis, T. (n.d.). Are Overdose Deaths Finally Peaking? Scientific American. Retrieved September 22, 2024, from https://www.scientificamerican.com/article/overdose-deaths-are-finally-starting-to-decline-heres-why/
Listos, J., Łupina, M., Talarek, S., Mazur, A., Orzelska-Górka, J., & Kotlińska, J. (2019). The Mechanisms Involved in Morphine Addiction: An Overview. International Journal of Molecular Sciences, 20(17), 4302. https://doi.org/10.3390/ijms20174302
Opioid Receptor—An overview | ScienceDirect Topics. (n.d.). Retrieved September 22, 2024, from https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/opioid-receptor
Opioid Use Disorder. (n.d.-a). Yale Medicine. Retrieved September 22, 2024, from https://www.yalemedicine.org/conditions/opioid-use-disorder
Shenoy, S. S., & Lui, F. (2024). Biochemistry, Endogenous Opioids. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK532899/
Wang, Y., Zhuang, Y., DiBerto, J. F., Zhou, X. E., Schmitz, G. P., Yuan, Q., Jain, M. K., Liu, W., Melcher, K., Jiang, Y., Roth, B. L., & Xu, H. E. (2023). Structures of the entire human opioid receptor family. Cell, 186(2), 413-427.e17. https://doi.org/10.1016/j.cell.2022.12.026
What Are Opioids? – Opioid Definition | Made for This Moment. (n.d.-a). Made For This Moment | Anesthesia, Pain Management & Surgery. Retrieved September 22, 2024, from https://madeforthismoment.asahq.org/pain-management/opioid-treatment/what-are-opioids/
About the author

Ankith Sureddi
Ankith is a current high school senior who wants to pursue a career in the medical field. At his high school, Ankith is in the Communications Arts Program on the Journalism and Debate Track. He is passionate about writing, science, and public health, leading him to find innovative ways to combine these passions by not only writing and researching medical and public health concepts that interest him but also by finding ways to communicate and disseminate that information to his peers.