Author: Jonathan Lu
Mentor: Dr. AbdelAziz Jalil
Concordia International School Shanghai
Abstract
Many treatments and therapies have been developed for treating cancer; however, these treatments suffer from serious side effects. Cancer vaccines are an innovation which manipulates the patient’s own immune system to specifically target their own cancer. The development of such therapies is critical in curing and preventing cancer. Tremendous research on cancer vaccines have been conducted over years, and several cancer specific vaccines have been approved by FDA since 1990. Even though an effective and universal cancer vaccine for all cancers does not currently exist, the recent progress on driver antigen cancer vaccines and targeted immunotherapy including CAR T-cell therapy and checkpoint inhibitor therapy show great promise. This review analyzes the feasibility of cancer vaccines and reviews some of the most recent advancements in this field.
Introduction
Cancer is a detrimental disease that has been recorded in humans as early as 1500 BCE. While there are plenty of treatment options for cancer patients, to this day no universal cure has been discovered. In 2021, more than 10 million people succumbed to cancer, with estimates of even more deaths in 2022. [28] Without any significant cure for this disease, millions of more lives will be taken each year. Cancer research is important as it helps doctors identify, cure, and prevent cancer, allowing people around the globe to have safer, longer, and higher quality lives. By understanding the biological processes of cancer, researchers can identify patterns which assist in developing ways to protect people from developing cancer and treating cancer patients. This will ultimately result in decreased occurrences of cancer and mortality. With the help of the research funding (USD 6.4 billion in 2020 alone), there have been many breakthroughs in cancer treatment. [2] One of these breakthroughs is called targeted immunotherapy, which is also known as the cancer vaccine. [3] This therapy uses the patient’s own immune system to destroy cancer. Although no complete cure has been fully developed, these cancer vaccines have been heavily researched and are used in patients. With cancer vaccines being one of the most prominent and potential cures to cancer in the future, this review briefly discusses the effects, processes, and results of cancer vaccines.
What is Cancer?
Cancer is a disease caused by an uncontrolled division of abnormal cells in parts of the body. There are many types of cancers such as breast, lung, colon, skin cancer, etc. As of 2022, breast cancer is the most common cancer in the US [12] whereas lung cancer is the most common cancer in China. [13] Statistics show that about 60% of people who are diagnosed with metastatic breast cancer also develop lesions in the lungs. [26] Metastatic cancers are when cancerous cells spread to another part of the body, which is commonly found in breast, colon, kidney, lung, among other cancers. An example of the metastasis can be seen in kidney cancer, where the cancer spreads to adrenal gland, bone, brain, liver, and lung.
Although cancer can develop and spread to different organs within the body, they share some similar symptoms such as fatigue, weight loss or gain, swelling, unusual bleeding or bruising, headaches, among many other symptoms. [34] The most severe symptoms usually are experienced by bone and pancreatic cancer patients. [33]
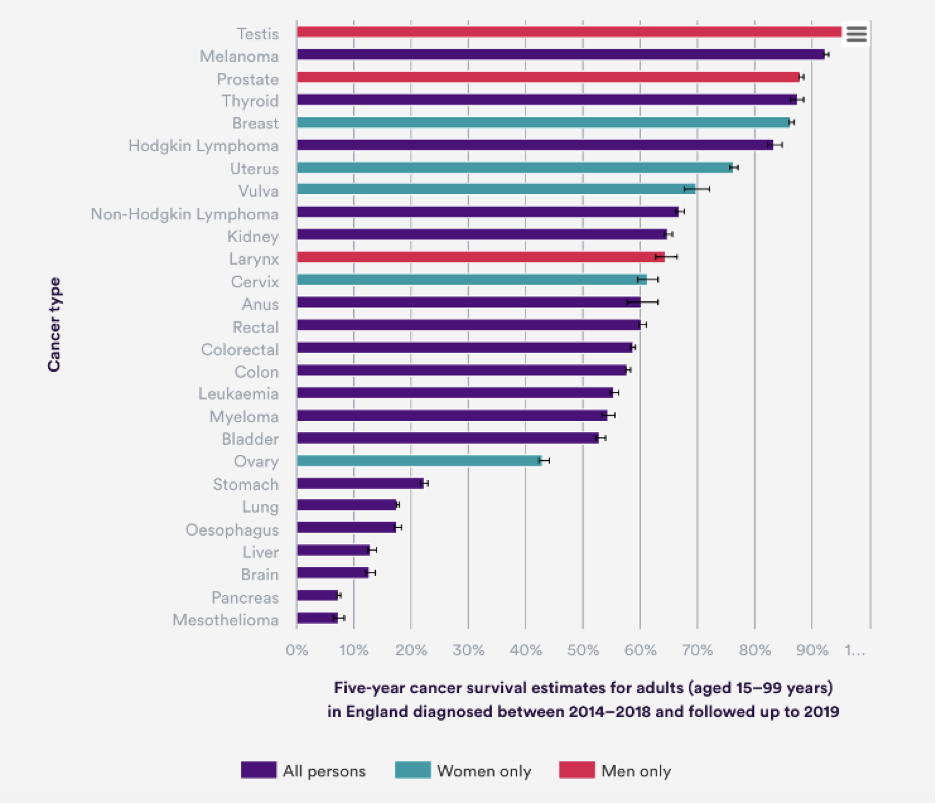
Figure 1: The 5-year survival rates for various types of cancers. (adapted from: www.nuffieldtrust.org)
In figure one, it shows that patients that are diagnosed with brain cancer usually have the lowest 5-year survival rates (12.8%) whereas testis cancer has the higher survival rate (97%) in England. [9] Interestingly, some cancer patients can live with their cancer as long as they continue treatment such as melanoma, breast, prostate, testicular, cervical, and thyroid cancer patients as the 5-year survival rates are highest.
http://www.bioch.ox.ac.uk/aspsite/index.asp?pageid=892
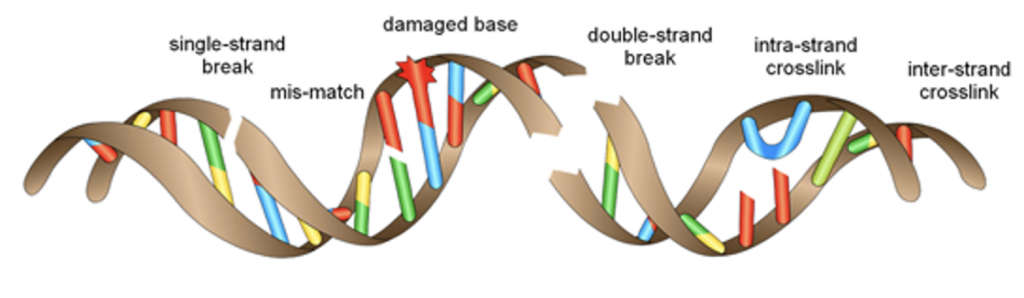
It is scientifically accepted that the universal cause of cancer is damage to genetic material i.e. DNA. Chemical disruption of the nucleotides that hold the DNA chains together results in genetic mutations once the DNA replicates itself. Loss or rearrangement of these nucleotides alters the genetic information contained in the DNA i.e. mutations. As can be seen in figure two, double strand breaks can also cause rearrangement of the chromosome structure, which could disrupt a gene and ultimately lead to mutation(s). However, these mutations can be avoided if the DNA repair system recognizes the DNA damage as abnormal structures and repairs it before the round of replication. [15] Alterations in DNA sequence result with improper cell cycle maintenance and functions. The sequence of DNA is important for expressing critical proteins in and on the cells of the body. When the sequence changes, that directly impacts the function of these proteins. Depending on where this damage occurs and which protein is affected, the function of the cell changes and can lead to developing cancerous cells.
There are a few exogenous factors that may cause DNA damage, and eventually cancer. These include lifestyle habits, such as, but not limited to, smoking, unhealthy diet, or exposure to toxic chemicals. DNA damage resulting from continuous smoking increases the chances for developing lung cancer, which can then spread to other parts of the body. [23] An unhealthy diet could lead a patient into obesity, which is a risk factor for various cancers such as colon, breast, kidney, etc. Maintaining a healthy body weight and also reducing alcohol intake can lower the risk of developing these cancers. [7] Exposure to heavy metals such as cadmium, arsenic, and nickel [18] (from factories or industrial productions), asbestos (aging and unmaintained buildings), and ultraviolet light (from the sun) can also cause damage to DNA in cells, leading to various cancers. There are many dangerous carcinogens such as PAH, N-nitrosamines, aromatic amines, 1,3-butadiene, benzene, aldehydes, and ethylene oxide which can cause damage to DNA. These carcinogens can be found in natural resources such as UV Light or viruses, or man-made waste like automobile fumes and cigarette smoke, and can cause mutations to the DNA, increasing the likelihood of cancer diseases. Some cancers can also be hereditary where one or both parents carry altered genes and carry that on to their offspring(s). Most common hereditary cancers are breast and colon. [37]
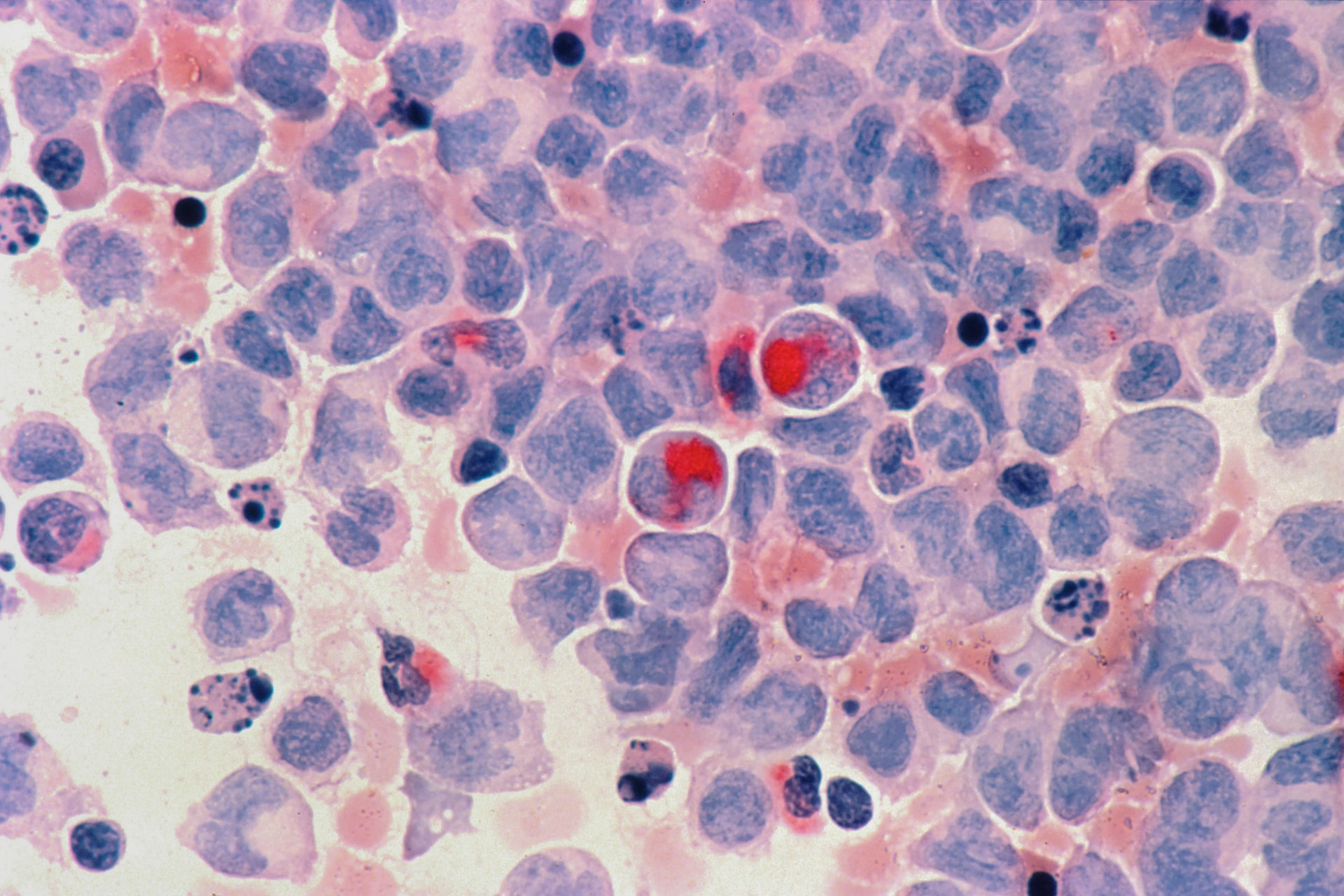
The main effect cancer has on the body is weakening of the immune system. For example, leukemia, lymphomas, and multiple myelomas spread into the bone marrow, outcompeting with the bone marrow cells for space and nutrients. [42] When this happens, the bone marrow won’t be able to generate white blood cells to fight infections in the body. Without a strong immune system, there is no protection against illnesses, leaving patients very vulnerable to other diseases. Not only do blood cancers affect the immune system, but also solid tumors. A tumor is a solid mass of tissue consisting of abnormal cell groups. Solid tumors grow on bones (sarcoma), skin (melanoma), lung (carcinoma), and other organs and glands. Malignant cells from the tumors avoid immune elimination through loss of antigenicity (ability to interact with immune cells and antibodies) and/or loss of immunogenicity (ability to provoke immune response). [24] The degree to which the tumor overrides the immune system on tumor type and lesion.
Many treatments have been developed to help cure or slow the progression of cancer. The most common treatments include surgery, chemotherapy, and radiation. [27] Surgery is the physical removal of a solid tumor/mass from the patient. Side effects of surgery include blood clots, bleeding, infections, damage of other organs, and reaction to drugs. [32] Chemotherapy is the use of drugs to kill cancer cells. Chemotherapy has negative side effects in which the immune system becomes weak, and infections are more probable. This is because chemotherapy is meant to kill fast growing cells, but they could also accidently affect healthy cells that are also fast growing. Radiation therapy uses x-rays, particles, or radioactive seeds to destroy the cancer. Radiation slows down the abnormal growth rate of the cancer cells. Side effects of radiation include fatigue, hair loss, memory or concentration problems, nausea, skin changes, and blurry vision. Most recently, targeted immunotherapy has been developed and considered to be the “cancer vaccine” for patients. This therapy focuses on using a person’s own immune system to fight cancer. The most prominent immunotherapies use CAR T-cell therapy and checkpoint inhibitors to fuel the production of cancer fighting cells to attack cancer cells. [41]
What Are Vaccines?
A vaccine is a substance used to stimulate the production of antibodies to provide long term immunity against a disease. The most common types of vaccines are live-attenuated vaccines, inactivated vaccines, and toxoid vaccines. Live-attenuated vaccines are created by using a weakened form of germ that causes the disease. These vaccines are similar to the natural infection, so it provides a strong and long lasting immune response. A limitation to this type of vaccine is people with weak immune systems, chronic health problems, and organ transplant recipients may not be eligible to receive such vaccines. Live-attenuated vaccines are used for various diseases including measles, rotavirus, smallpox, chickenpox, and yellow fever.
Inactivated vaccines use the deactivated version of the germ that causes the disease. The inactivated vaccines are not as strong or long lasting as the live-attenuated vaccines. This type of vaccine is a safer alternative for those with weak immune systems and chronic health problems since they are weaker than the live-attenuated vaccines. Booster shots are required for inactivated vaccines to ensure that the patient gets longer immunity against diseases. Inactivated vaccines are used for hepatitis A, flu, polio, and rabies. Toxoid vaccines use a toxin made by the germ that causes the disease. It creates immunity against the germs that cause the disease, but not the disease itself. Similar to the inactivated vaccine, it also requires booster shots for an ongoing immunity against diseases. Toxoid vaccines are used to protect against diphtheria and tetanus. [40]
With the outbreak of the COVID-19 pandemic, a new type of vaccine has been developed and globally used to prevent the spread of this deadly virus and maintain the lives of billions. These vaccines are mRNA based, which means inactivated regions of proteins from the virus are genetically encoded to be expressed on the surface of healthy cells. Once these proteins are detected by the immune cells, an immune response is generated. The main difference compared to the vaccine types above is that these proteins remain on the surface of the cells as long as the cells are in the body. [29] This method has been researched for more than a decade but has only been used in humans since the pandemic outbreak. Given that this technology is still in its infancy, there are many areas of development to increase the efficiency and longevity of mRNA vaccines.
Innovating Vaccines against Cancer
Cancer has always seemed to be the greatest enigmas of the modern day as no universal cure has been developed. The idea of a cancer vaccine – not a direct cure, but a prevention against cancer – is an absolute breakthrough as it has the potential to drastically decrease the mortality and infection of cancer throughout the globe. Unlike the types of vaccine mentioned in the last section, cancer vaccines take advantage of proteins found in or on cancer cells. [41]
The progress to the current cancer vaccines in early trials has come a long way. Immunotherapy was first developed in 1891 by William Coley, also known as the “father of immunotherapy.” Coley attempted to leverage the immune system through injecting patients with bacteria or bacterial products. His belief was that forcefully activating the immune system will generate a response against inoperable cancers. While his approach was not entirely understood or accepted by professionals and healthcare providers at the time, he was able to treat about 1000 cases of bone and soft-tissue sarcoma where patients’ tumors decreased in size after being injected with these inactivated bacteria. These short lived, “immunotherapy” injections were referred to as Coley Toxins. [39]
About a century later, the first FDA approved cancer vaccine (1990) was BCG (Bacillus Calmette-Guérin) which uses a weakened strain of TB (tuberculosis) bacteria, and it triggers the immune system to protect against the infection that results in early-stage bladder cancer. [6, 10] A second FDA approved cancer vaccine (2010) is the Sipuleucel-T, which is an autologous cellular immunotherapy used for patients with metastatic castration-resistant prostate cancer (mCRPC). The vaccine activates the multiplication of immune cells and attacks prostate cancer cells using an antigen (one or more proteins on the surface of cancer cells that induce an immune response), that is highly specific to prostate cancer. [16, 8] A third FDA (2015) approved cancer vaccine is called T-VEC (Talimogene laherparepvec). T-VEC is an immunotherapy for treatment of melanoma skin cancer. T-VEC is made with a weakened version of herpesvirus in which it can break down cancer cells without affecting normal cells. Unlike other cancer vaccines, T-VEC is injected directly into the tumor. [38]
While two of the three cancer vaccines mentioned primarily function on established tumors/cancers, the more traditional way of thinking about vaccines is to prevent the disease from occuring. Since cancer is a genetic-based disease for the most part, this has been the greatest challenge in developing immune-shields against cancer. However, there are some “traditional” vaccines that immunize against viruses known to be linked to development of cancer. Epstein-Barr virus (EBV) is linked to nasopharyngeal cancer, stomach cancer, and Bukitt/Hodgkin lymphoma. The EBV vaccine targets EBV glycoprotein gp350, which is found in the virus and on virus infected cells. Gp350 is the main target for neutralizing antibodies in the body and causes cells to target a specific antigen. [31] Human papillomavirus (HPV) causes most cervical cancers including vulva, vagina, penis, anus, and oropharynx cancer. [5] The HPV vaccine is a non-infectious recombinant vaccine that stimulates the body to produce antibodies. These antibodies bind to specific parts of the HPV and signal to the immune cells to destroy these virus particles, preventing viral infection. Hepatitis B virus (HBV) causes chronic hepatitis, liver cirrhosis, and hepatocellular carcinoma. [21] The HBV vaccine is also a recombinant vaccine and it work by causing the body to produce its own antibodies against the disease. [20,19] Human herpes virus (HSV) has been linked to cause cervical cancer. [22] While there aren’t any approved vaccines against HSV, there is a potential mRNA-based vaccine that is being studied to prevent HSV. The concept of this vaccine is to provide a strong antibody response and drive immune cells to kill HSV particles. [30, 14]
Many years of commitment have been put into developing immune cell-based therapies. Although there were many obstacles in developing and implementing this therapy, immune cells that were engineered to treat cancer called CAR T cells (approved by the FDA in 2017 and created by Novartis) were discovered. CAR T cells, also known as chimeric antigen receptor T cells, have been implemented in cancer treatment including lymphomas, leukemia, and myelomas. CAR T-cells are referred to as a living drug as they orchestrate the immune system and directly kill pathogenic cells. Immune T cells are harvested from patients and are customized for each patient. This results with highly engineered CAR T cells that can recognize and bind to specific proteins or antigens on the patient’s own cancer cells prompting their elimination. These T cells are customized because normal T cells are incapable of binding to these antigens. Once these cells are injected, they are directed towards cancer cells that express the antigen the CAR is designed to target. One major drawback is that since cancer cells are abnormal human cells, these antigens are sometimes expressed on healthy cells leading to off-target toxic effects. Not only are CAR T cells referred to as a cancer therapy, but they can also be considered a vaccine because the cells remain in circulation and proliferate inside the patient, potentially protecting against any recurrence of the cancer. [11]
In 2022, researchers believe they have found another viable cancer vaccine based on positive clinical trial results. Olivera Finn, a professor of immunology at the University of Pittsburgh was able to identify a colon tumor-specific antigen known as MUC1. Finn’s team was able to create a MUC1-based vaccine to help patients with premalignant colon polyps. This vaccine works by triggering an immune system response to attack the colon polyps. The vaccine reduced recurrence rates by 38% in the clinical trial, proving its effectiveness. Another example of the use of an antigen is the HER2, which is a protein found in about 25% of breast cancers. Knutson and Amy Degnim, who are breast surgeons at Mayo Clinic in Minnesota designed a HER2 vaccine used in a trial of 22 patients with invasive breast cancer. This vaccine is like the MUC1 vaccine where it targets the antigen, provokes the immune system, and kills cancer cells. The results were very promising, with only two recurrences after two years. [11] Although the timetable for a truly universal cancer vaccine is unclear, these examples of clinical trials show the potential of these vaccines to cure cancer, and how researchers are setting the stage to make cancer history. [1]
Conclusion
The most prominent method that researchers have been developing these cancer vaccines is using “driver” antigens, which acts as a target for the immune system. Although these cancer vaccines seem promising, a limitation is that tumors express an array of antigens that are also common in healthy cells, making it difficult for researchers to identify tumor-specific antigens. Cancer vaccines are not like live-attenuated or inactive vaccines where the germ is already placed in the body. Rather, they use these antigens to make the immune system purposely attack the tumors to prevent recurrence. Cellular immunotherapies introduce the least risk of toxic side effects since the cells are from the patient and they are engineered to target the cancer specifically. Similar to CAR-T therapy, researchers have developed CAR-macrophages (CAR-M) where these immune cells are also engineered in a similar manner to CAR-T cells. [17] However, a unique method to activate macrophage immune cells is to use antibodies, proteins and peptides to block interactions responsible for survival of the cancer cells and then only have activating signals against the cancer. [4] This is also known as checkpoint inhibitor therapy. Many breakthroughs along the studies of a cure for cancer have arisen recently, and it may just be a matter of a few years before the deadliest disease is eradicated.
References
[1] (2022, June 14). Retrieved from https://www.washingtonpost.com/health/2022/06/14/cancer-vaccine-future/
[2] 2021 NCI budget fact book – Research funding. (n.d.). Retrieved from https://www.cancer.gov/about-nci/budget/fact-book/data/research-funding
[3] 5 Oncology Breakthroughs to be Excited About in 2022. (2022, May 11). Retrieved from https://www.cityofhope.org/breakthroughs/5-oncology-breakthroughs-to-be-excited-about-in-2022
[4] Activated macrophages in the tumour microenvironment – dancing to the tune of TLR and NF-κb. (n.d.). Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2935674/
[5] Basic information about HPV and cancer. (2021, December 14). Retrieved from https://www.cdc.gov/cancer/hpv/basic_info/
[6] BCG vaccine for tuberculosis (TB) overview. (2019, 31). Retrieved from https://www.nhs.uk/conditions/vaccinations/bcg-tuberculosis-tb-vaccine/
[7] Cancer and food. (n.d.). Retrieved from https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/cancer-and-food
[8] Cancer, C. C. (n.d.). Sipuleucel-T – Chemotherapy drugs – Chemocare. Retrieved from https://chemocare.com/chemotherapy/drug-info/SipuleucelT.aspx
[9] Cancer survival rates. (2022, June 29). Retrieved from https://www.nuffieldtrust.org.uk/resource/cancer-survival-rates
[10] Cancer vaccines: Preventive, therapeutic, personalized. (n.d.). Retrieved from https://www.cancerresearch.org/en-us/immunotherapy/treatment-types/cancer-vaccines
[11] CAR T cells: Engineering immune cells to treat cancer. (2022, March 10). Retrieved from https://www.cancer.gov/about-cancer/treatment/research/car-t-cells
[12] Common cancer types. (2022, May 10). Retrieved from https://www.cancer.gov/types/common-cancers
[13] Comparison of cancer incidence between China and the USA. (n.d.). Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3643656/
[14] Developments in vaccination for herpes simplex virus. (n.d.). Retrieved from https://www.frontiersin.org/articles/10.3389/fmicb.2021.798927/full
[15] DNA damage, DNA repair and cancer. (n.d.). Retrieved from https://www.intechopen.com/chapters/43929
[16] Factors associated with use of Sipuleucel-T to treat patients with advanced prostate cancer. (n.d.). Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6481456/
[17] First-in-Human trial with CAR macrophages shows the cell therapy may be safe, feasible for solid tumors – Penn medicine. (n.d.). Retrieved from https://www.pennmedicine.org/news/news-releases/2022/january/first-in-human-trial-with-car-macrophages-shows-the-cell-therapy-safe-feasible-for-solid-tumors
[18] Heavy metal exposure influences double Strand break DNA repair outcomes. (n.d.). Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4788447/
[19] Hepatitis B vaccination. (2022, May 5). Retrieved from https://www.cdc.gov/vaccines/vpd/hepb/index.html
[20] Hepatitis B vaccine (Intramuscular route) description and brand names – Mayo Clinic. (2022, February 14). Retrieved from https://www.mayoclinic.org/drugs-supplements/hepatitis-b-vaccine-intramuscular-route/description/drg-20068700
[21] Hepatitis B virus and cancer prevention. (n.d.). Retrieved from https://pubmed.ncbi.nlm.nih.gov/21253790/
[22] Herpes simplex virus. An expanding relationship to human cancer. (n.d.). Retrieved from https://pubmed.ncbi.nlm.nih.gov/6300393/
[23] How does smoking cause cancer? (2021, March 19). Retrieved from https://www.cancerresearchuk.org/about-cancer/causes-of-cancer/smoking-and-cancer/how-does-smoking-cause-cancer
[24] Immune escape mechanisms as a guide for cancer immunotherapy. (15, February). Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4334715/
[25] Immunotherapy: Cancer treatment, CAR T-cell therapy, types, risks. (n.d.). Retrieved from https://my.clevelandclinic.org/health/treatments/11582-immunotherapy
[26] Lung metastasis. (n.d.). Retrieved from https://www.breastcancer.org/types/metastatic/lung-metastasis
[27] MedlinePlus: We’re sorry, we can’t find the page you requested. (n.d.). Retrieved from https://medlineplus.gov/ency/patientinstructions/000901.html
[28] Morgan, K. K. (2020, May 20). How many people die of cancer a year? Retrieved from https://www.webmd.com/cancer/how-many-cancer-deaths-per-year
[29] MRNA vaccines — a new era in vaccinology. (2018, January 12). Retrieved from https://www.nature.com/articles/nrd.2017.243
[30] Mrna-1608 herpes vaccine. (2022, February 18). Retrieved from https://www.precisionvaccinations.com/vaccines/mrna-1608-herpes-vaccine
[31] NIH launches clinical trial of Epstein-Barr virus vaccine. (2022, May 6). Retrieved from https://www.niaid.nih.gov/news-events/nih-launches-clinical-trial-epstein-barr-virus-vaccine
[32] Risks of cancer surgery. (n.d.). Retrieved from https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/surgery/risks-of-cancer-surgery.html
[33] Seladi-Schulman, J. (n.d.). Most painful cancer: What to know about pain and treatment. Retrieved from https://www.healthline.com/health/cancer/most-painful-cancer
[34 Signs and symptoms of cancer. (n.d.). Retrieved from https://www.cancer.org/treatment/understanding-your-diagnosis/signs-and-symptoms-of-cancer.html
[35] SIRPA-inhibited, marrow-derived macrophages engorge, accumulate, and differentiate in antibody-targeted regression of solid tumors. (n.d.).
[36] Suppressing or Enhancing Macrophage Engulfment through the Use of CD47 and Related Peptides. (n.d.). Retrieved from https://www.sciencedirect.com/org/science/article/abs/pii/S1043180222004256
[37] Table of different genes and the hereditary cancers that they cause. (n.d.). Retrieved from https://www.facingourrisk.org/info/hereditary-cancer-and-genetic-testing/genes-by-cancer-types
[38] Talimogene Laherparepvec (T-VEC). Retrieved from https://www.cancerresearchuk.org/about-cancer/cancer-in-general/treatment/cancer-drugs/drugs/talimogene-laherparepvec
[39] The Toxins of William B. Coley and the Treatment of Bone and Soft-Tissue Sarcomas. (n.d.). Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888599/
[40] Vaccine types. (2021, December 6). Retrieved from https://www.hhs.gov/immunization/basics/types/index.html
[41] Vaccines to treat cancer. (n.d.). Retrieved from https://www.cancerresearchuk.org/about-cancer/cancer-in-general/treatment/immunotherapy/types/vaccines-to-treat-cancer
[42] Why people with cancer are more likely to get infections. (n.d.). Retrieved from https://www.cancer.org/treatment/treatments-and-side-effects/physical-side-effects/low-blood-counts/infections/why-people-with-cancer-are-at-risk.html
About the author

Jonathan Lu
Jonathan Lu is a senior at the Concordia International School in Shanghai, China. Jonathan has a passion for Physics, Materials Science, Chemistry, Engineering, Biology, and all things basketball. In the paper, Jonathan analyzes the development of cancer vaccines and immunotherapy.