Author: Sophia Zhang
Shanghai American School
November 1, 2021
“I think I have OCD because I want everything to be neat.”
Obsessive-Compulsive Disorder is one of the most well-known mental illnesses. However, it’s also one of the most misunderstood. Often when someone says, “I think I have OCD,” they’re referring to the fact that they always like to keep things organized. This, however, is not true. OCD symptoms consist of obsessing over the tiniest things. The obsession leads to constant anxiety and crushing stress. It’s not just someone wanting everything to be neat. People with OCD face repeated intrusive thoughts that mix with fear or danger. [1]
The fear that envelopes those with OCD can materialize as a need for symmetrical arrangement, although everyone’s symptoms differ based on their doubts in themselves and other internalized concerns. People who genuinely have OCD do not simply engage in excessively detailed practices because they feel like it. They constantly have these compulsions because of the anxiety that’s weighing on them; for example, the constant need to check on their family members or loved ones to make sure that they’re safe. [2]
According to www.helpguide.org, the cycle of OCD includes 1; an obsessive thought taking over someone’s mind. 2; the anxiety that comes along with not being able to control the thought. 3; compulsive behaviors such as repeatedly tapping or touching an object. 4; the temporary relief. Upon reaching the final step, the cycle starts again. These continued thoughts are what makes OCD such a severe illness and not something to joke about. [2] Patients who have it describe it as a ‘mental discomfort’ that leads to anxiety and fear. [5]
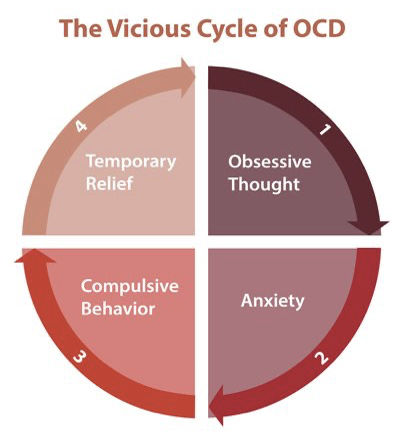
Note: This is the cycle of OCD involving the different stages that a patient goes through in order to get rid of an obsessive thought.
Image from: https://www.helpguide.org/articles/anxiety/obssessive-compulsive-disorder-ocd.htm#:~:text=Common%20compulsive%20behaviors%20in%20OCD,senseless%20things%20to%20reduce%20anxiety.
Simply because someone prefers everything to be neat does not mean that they have OCD. This common misconception can lead to others believing that this illness is not as severe and profound as it truly is. Bystanders will think that it is okay to use the term “OCD” lightly.
When people see the symptoms and effects of OCD, they start to say things such as, “calm down, nothing bad will happen,” or, “the stove is off, don’t recheck it, it’s fine.” [3]However, for someone who truly suffers from OCD, these obsessions cannot just be cured by “calming down.” This is a severe chronic illness that deserves more attention. These obsessions and compulsions are almost outright impossible to control without medical help. [3] The thought itself is caused by a disturbance between the frontal cortex of one’s brain and the ventral striatum. Patients cannot just “calm down” when in the cycle of OCD because it is near impossible to control their anxiety. [4]
My research aims to identify the frequency of misinterpretation of OCD as well as the adverse effects that such misinterpretation may cause on those who have OCD. My study analyzes existing data on the prevalence of OCD, including self-developed surveys of individuals with and without OCD.
How OCD is Mischaracterized
Having OCD misinterpreted is extremely disrespectful to actual patients suffering from the disorder. Over 1 percent of Americans suffer from OCD. [6] Yet around 66% of Americans say that a dirty home makes them feel anxious.[7] These two types of anxiety are completely different. While OCD is a serious mental illness affecting 2.2 million Americans, feeling anxious about a dirty home is a common anxiety shared among over half of the population. There are so many people among these patients who hide their symptoms from embarrassment or fear. [8] Joking about OCD is extremely disrespectful and embarrassing to those who suffer from the illness. Saying “I’m so OCD” can blur the line between a devastating disorder and a regular need for neatness. People are stripping the illness of its severity, and this also applies to any illness. This can make it extremely hard for people to seek help. [9]
Making light of this extremely serious mental illness is not only insensitive, but extremely detrimental to a patient. Those with OCD might feel as though their very real symptoms and obsessions aren’t as important, leading them to avoid seeking help. Making a joke of OCD, or saying that one has it is making fun of an extremely tortuous routine that patients have to go through daily. Those who mischaracterize OCD are contributing to the stigma that has made many patients hide their illness for years and years. People are joking about patients who have to go through exhausting rituals as well as intrusive thoughts just to sound “quirky and different.” [8]
There are multiple scenarios where people mischaracterize OCD. The seven main ones include: Keeping a tidy living space, worrying about an upcoming event, wanting to arrive somewhere early, being a “perfectionist,” wanting to wash one’s hands, hanging onto things one doesn’t use anymore, and finally checking and then double-checking things. [10] Each of these examples are common anxieties among people who don’t have OCD. All of these things might annoy or bug someone, but it’s not to the extent of OCD, and it doesn’t have as negative of an impact on people, says a licensed psychologist Dr. Crystal I. Lee. [10]
A lot of things that annoy the usual person doesn’t affect them the same way as an obsession would affect a patient with OCD. OCD is much more extreme and it takes up so much more time in a patient’s life. The reason why OCD is so mischaracterized is because of the lack of education. Most people don’t easily come across information on certain illnesses because it doesn’t affect them, and they don’t search it up. OCD is also extremely misportrayed in the media. There’s a false representation of the mental illness. It’s usually represented mainly around a fear of germs and cleaning compulsions. When the majority of people look at the media and see this, it doesn’t give a clear picture of OCD. They feel like OCD is just what the media portrays it as. [11]
What It Truly Means to Have OCD
Charlotte, an anonymous contributor to the mental health awareness website www.mind.org, says OCD is like a constant fear of not being able to complete something the right way. She lives with obsessions taking over her thoughts daily. He also has rituals to get rid of those obsessions, which are called compulsions. She says that these compulsions are extremely horrific, especially because she has these thoughts on a daily basis. [12] Imagine having unwanted thoughts up to 20 times a day, and not being able to get rid of them.
Mark Highet, a father and public servant from Queensland, Australia, says that even everyday actions like turning on a light switch can trigger his OCD. This can lead to anxiety, causing him to do rituals in order to forget about the obsessions. “For example, one day I was filling up my daughter’s water bottle,” he says, “and I had the thought that the water might be contaminated. I rationally knew it wasn’t, but I had this worry. So, I turned back to the sink, tipped it out and filled it again. I went to give it to her, but then I worried again, so I tipped it back out. I must have done it 40 times.” Mark goes on to say that it almost feels humiliating when someone from work sees him doing a ritual. He says that it feels like he’s so busy trying to live, that he’s forgetting to live. [13]
OCD isn’t just wanting everything to be neat. It’s about spending minutes to hours of one’s day trying to get rid of a thought that’s taking over one’s mind. For some, it might be “if I don’t do this, my family is going to get hurt.”[9] For others, it might be “If I turn something on, I might not be able to turn it off.” [13] These thoughts cause extreme and heavy anxiety among patients who have OCD. It can cause them to fear for their loved ones, because they think that they’ll end up hurting someone close to them. These thoughts aren’t just shallow little ‘what ifs.’ They are thoughts that can significantly impact a person’s life. It’s extremely complex, far past the point of wanting everything to be perfect. OCD can cause an overload of function systems in one’s brain. [14]
Having a constant obsession on one’s mind can lead to rituals. Rituals are an action that a patient performs when they try to forget about the obsession taking over their mind. For example, performing a repetitive activity, like locking, unlocking, and relocking a door. These rituals are usually performed physically to get rid of the muscle tension coming from obsessive thoughts. Rituals are usually described as mental and physical exercises that people with OCD perform to get rid of feelings such as disgust or anxiety. Rituals can also be performed to prevent a dangerous situation. People with OCD often can’t suppress their thoughts, which is why they cope through performing rituals. [15] Hattie Gladwell from metro.co.uk says that OCD takes up around 14 hours of her week every single week. [16] That’s over 8% of her entire week. These rituals aren’t actions that can be done only one or two times and solved. Patients spend hours and hours trying to get rid of their obsessions.
Dangers of Mischaracterization
Charlotte at Mind.org also mentions, “anyone who says that having OCD is ‘helpful’ couldn’t be further from the truth. I may spend hours cleaning dishes and making sure my things are organised/symmetrical – but when will any of these compulsions benefit me? NEVER.” [12] Saying that OCD is beneficial to patients is disrespectful in and of itself because one is making a really serious mental illness seem like it’s benefiting a patient, even if in reality, it’s hurting them.
Mark Highet has experienced jokes about OCD firsthand. He says, “At my work we have a regular meeting, where everyone goes around the table and updates on how they’re going. One day, one of my co-workers said, ‘Oh sorry, that’s so OCD of me,’ when she finished her bit. When I hear that, I think, ‘if only you knew.’ It’s a real, and really hard, condition.” Jokes like this can increase the stigma around OCD itself, which is harmful to people who are seeking help. It’s a real mental health issue, and no laughing matter. Michelle Blanchard says that “OCD is often appropriated as a casual term but trivialising it only adds to the stigma that often prevents people from seeking help.” [13]
Serena Ata from the website inkspire.org says that she wasn’t able to fully diagnose her OCD because of the stigma around the disorder. All of her symptoms were viewed as “normal” because people said that all her compulsions were things that she would grow out of. Serena says that making jokes about OCD is extremely damaging to patients who suffer from the disorder. For her, she had to spend years scrolling through the internet to try and find an answer and a reason as to why she was spending hours of her week on rituals. “Unfortunately, many sufferers find themselves dependent on unreliable platforms for answers, often leading to a vicious cycle of misinformation, misunderstanding and misdirection.” [17]
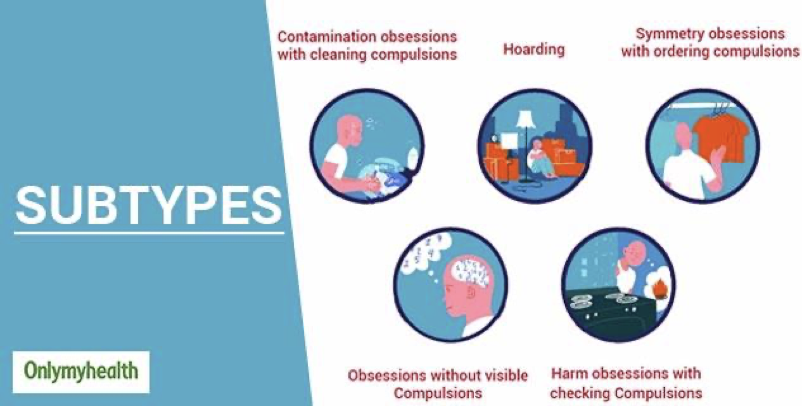
Note: This visual represents several common ways in which OCD manifests itself in patients.
Image from: https://www.onlymyhealth.com/obsessive-compulsive-disorder-ocd-symptoms-treatment-diagnosis-1595417322
It can take up to 17 years on average for people to receive an OCD diagnosis. [18] Only about 200,000 people with OCD seek therapy out of the 4.1 million people who need the treatment. [19] When patients view the media and see OCD being portrayed as a simple little quirk, they won’t seek out help, and they won’t try to get treatment. Patients would feel like their symptoms are normal, and they put it aside. Mischaracterizing OCD can lead to actual patients taking years and years to seek the treatment that they actually need. This can harm the patients themselves, because OCD symptoms can progressively get more intense. OCD symptoms get worse with age, so when patients don’t seek help at a young age, it would be harder for them to deal with it. [20]
Conclusion and Further Guidance
Mischaracterizing OCD can lead to patients not getting correct treatment, and patients feeling like their mental illness isn’t actually serious. It harms the OCD community by joking about a mental illness that’s extremely legitimate. Mischaracterizing OCD can also add to the stigma around the topic. When the media portrays OCD as something light and fun, it can lead to patients feeling like their symptoms aren’t important, even though they are. If any individuals have ever made a joke about OCD or have mischaracterized OCD, they should do their best to educate themselves on the topic. One should start to take this disorder more seriously from now on, and do one’s best to support patients with OCD as best as they can.
If someone knows a family member or friend who has OCD, the Victoria State Government Department of Health recommends that one should first make sure to educate themselves on their family member’s disorder. When people have connections with patients, it can ease the tension around their relationship. When they’re performing a ritual, one shouldn’t participate in the rituals themselves, because it could reinforce OCD behaviour and it could lead to symptoms potentially getting worse. [21] Though one shouldn’t assist them in the rituals themselves, they should remind them that it shouldn’t be something that they’re embarrassed about. They should make sure that they’re getting the right treatment like professional help.
In the event that a patient starts to lose motivation in seeking help, close relatives and friends should continue supporting them. If they start to have less motivation to go get treatment, studies say that individuals should make sure that they remind patients about the progress that they’ve made through the whole process. Seeking help isn’t a sign of weakness, it’s a sign of strength. [21] It shows that they’re trying to treat their disorder. The general public can also help with maintaining a non-judgemental attitude, which can help as well, because patients know that their obsessions are irrational. Finally, the Victoria Department of Health recommends encouraging patients and rewarding them for the gains they’ve made. Most importantly, accept patients for who they are, and don’t ridicule them for their rituals. Supporting a patient with OCD is the best thing to do when they’re going through a difficult time.
Works Cited:
[1] Benenden Health. (n.d.). OCD: Myths vs Reality. Benenden Health. Retrieved May 7, 2021, from https://www.benenden.co.uk/be-healthy/mind/ocd-myths/
[2] Smith, M., Robinson, L., & Segal, J. (2021, February). Obsessive-Compulsive Disorder (OCD). Help Guide. Retrieved May 7, 2021, from https://www.helpguide.org/articles/anxiety/obssessive-compulsive-disorder-ocd.htm#:~:text=Common%20compulsive%20behaviors%20in%20OCD,senseless%20things %20to%20reduce%20anxiety.
[3] Ryback, R. (2016, May 9). 4 Myths About OCD. Psychology Today. Retrieved May 7, 2021, from https://www.psychologytoday.com/us/blog/the-truisms-wellness/201605/4-myths-about-ocd
[4] Pronghorn Psych. (n.d.). How Obsessive Compulsive Disorder Affects the Brain. Stone Ridge. Retrieved May 7, 2021, from https://pronghornpsych.com/how-ocd-affects-the-brain/#:~:text=Researchers%20know%20that%20obsessive%2Dcompulsive,known%20as%20 the%20ventral%20striatum
[5] Mind. (2019, May). Obsessive-compulsive disorder (OCD). Mind. Retrieved May 7, 2021, from https://www.mind.org.uk/information-support/types-of-mental-health-problems/obsessive-compulsive-disorder-ocd/about-ocd/
[6] ADAA. (2021, October). Facts & Statistics. Anxiety and Depressions Association of America. Retrieved May 18, 2021, from https://adaa.org/understanding-anxiety/facts-statistics#:~:text=Crisis%20(Oct%202020)-,Obsessive%2DCompulsive%20Disorder%20(OCD) ,cases%20occurring%20by%20age%2014.
[7] Heinz, A. (2019, October 7). Survey: Americans More Annoyed With Clutter Than Dirt. Apartmentguide. Retrieved May 18, 2021, from https://www.apartmentguide.com/blog/americans-annoyed-with-clutter/
[8] George, N. (2014, September 3). When It’s Not Just OCD. Everyday Health. Retrieved May 10, 2021, from https://www.everydayhealth.com/news/when-its-not-just-ocd/?pos=2&xid=nl_EverydayHealthMentalHealthandMoodDisorders_20171015
[9] Gallagher, W. (2017, October 23). You’re Actually Not “So OCD,” And Here’s Why You Shouldn’t Joke About It. Rolling Hills Hospital. Retrieved May 10, 2021, from https://rollinghillshospital.org/youre-actually-not-ocd-heres-shouldnt-joke/#:~:text=Unfortunately%2C%20for%20about%202.2%20million,OCD%20is%20no%20laughing %20matter.&text=You%20may%20not%20realize%20it,who%20deals%20with%20the%20disorder
[10] Steber, C. (2018, January 30). 7 Symptoms That Are Wrongly Mistaken As OCD. Bustle. Retrieved May 19, 2021, from bustle.com/p/7-symptoms-that-are-wrongly-mistaken-as-ocd-8026866
[11] D’Arcy-Sharpe, A.-M. (2020, January 6). Why Is OCD So Misunderstood And Misdiagnosed? IMPULSE. Retrieved May 19, 2021, from https://impulsetherapy.com/why-is-ocd-so-misunderstood-misdiagnosed/
[12] Charlotte. (2016, June 23). Living with OCD. Mind. Retrieved May 7, 2021, from https://www.mind.org.uk/information-support/your-stories/living-with-ocd/
[13] Queensland Health. (2018, October 10). What is it like to live with obsessive compulsive disorder? Queensland Government. Retrieved May 11, 2021, from https://www.health.qld.gov.au/news-events/news/living-with-obsessive-compulsive-disorder-OCD-symptoms-treatment-Queensland
[14] International OCD Foundation. (2016, October). OCD – Misunderstood and Misdiagnosed | Orlando OCD Therapist Raises Awareness #OCDWEEK. Ground Work Counseling. Retrieved May 11, 2021, from https://www.groundworkcounseling.com/ocd/ocd-misunderstood-and-misdiagnosed-orlando-ocd-therapist-raises-awareness-ocdweek/#:~:text=A%20misdiagnosis%20of%20OCD%20has,management%2C%20 hospitalization%20and%20inaccurate%20reporting.
[15] Pulse. (n.d.). OCD Rituals: Symptoms and Treatment Options. Pulse. Retrieved May 11, 2021, from https://pulsetms.com/ocd/rituals/
[16] Gladwell, H. (2018, January 26). How much time OCD rituals take out of my day-to-day life. METRO. Retrieved May 19, 2021, from https://metro.co.uk/2018/01/26/how-much-time-ocd-rituals-take-out-of-my-day-to-day-life-7259595/
[17] Ata, S. (2020, November 2). “So OCD”: The Consequences of Delegitimizing a Disorder. INKSPIRE. Retrieved May 19, 2021, from https://inkspire.org/post/so-ocd-the-consequences-of-delegitimizing-a-disorder/-MHg9RS6V1RColwvc–S
[18] NOCD Staff. (2020, December 15). How Long Does OCD Treatment Take? NOCD. Retrieved May 19, 2021, from https://www.treatmyocd.com/blog/how-long-does-ocd-treatment-take
[19] Gershkovich, M., Middleton, R., Hezel, D. M., Grimaldi, S., Renna, M., Basaraba, C., Patel, S., & Simpson, H. B. (2020). Integrating Exposure and Response Prevention With a Mobile App to Treat Obsessive-Compulsive Disorder: Feasibility, Acceptability, and Preliminary Effects. ScienceDirect. Retrieved May 19, 2021, from https://www.sciencedirect.com/science/article/abs/pii/S0005789420300666
[20] Penn Psychiatry. (n.d.). OCD: SOME FACTS. Perelman School of Medicine. Retrieved May 19, 2021, from https://www.med.upenn.edu/ctsa/forms_ocdfacts.html#:~:text=Symptoms%20fluctuate%20in%20 severity%20from,symptoms%20were%20disrupting%20their%20lives.
[21] Obsessive compulsive disorder – family and friends. (n.d.). BetterHealth. Retrieved May 27, 2021, from https://www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/obsessive-compulsive-disorder-family-and-friends
[22]Dogra, T. (2020, July 22). Obsessive-Compulsive Disorder (OCD): Symptoms, Treatment And Diagnosis. Onlymyhealth. Retrieved June 1, 2021, from https://www.onlymyhealth.com/obsessive-compulsive-disorder-ocd-symptoms-treatment-diagnosis-1595417322
About the author

Sophia Zhang
Sophia is a student at the Shanghai American School – Puxi Campus.