Author: Joanne Lin
Mentor: Dr. Amy Abruzzi
Maggie L. Walker Governor’s School
Abstract
The connection between socioeconomic status and health has long been acknowledged, but the close examination of the effect that one’s food environment has on their health is a more recent phenomenon. The purpose of this paper is to discuss food desserts and their health outcomes as a hurdle to health equity and public health, especially in Richmond City, Virginia. Richmond City has been identified as one of the largest food deserts in the country for a city of its size (Jake Burns, 2015). Additionally, this paper evaluates various strategies that have been undertaken and/or proposed to alleviate these obstacles and considers the effectiveness of each. Feasibility, effectiveness, and sustainability of the strategies were considered as part of this evaluation. The results of this research concluded that the most effective short-term solution would be to incentivize farmers’ markets in low-income areas, and the most effective long-term solution being incentivizing the development of supermarkets in low-income areas.
Keywords: food deserts, food access, supermarkets, grocery stores, health equity, low-income communities, diabetes
Food Deserts and their Implications
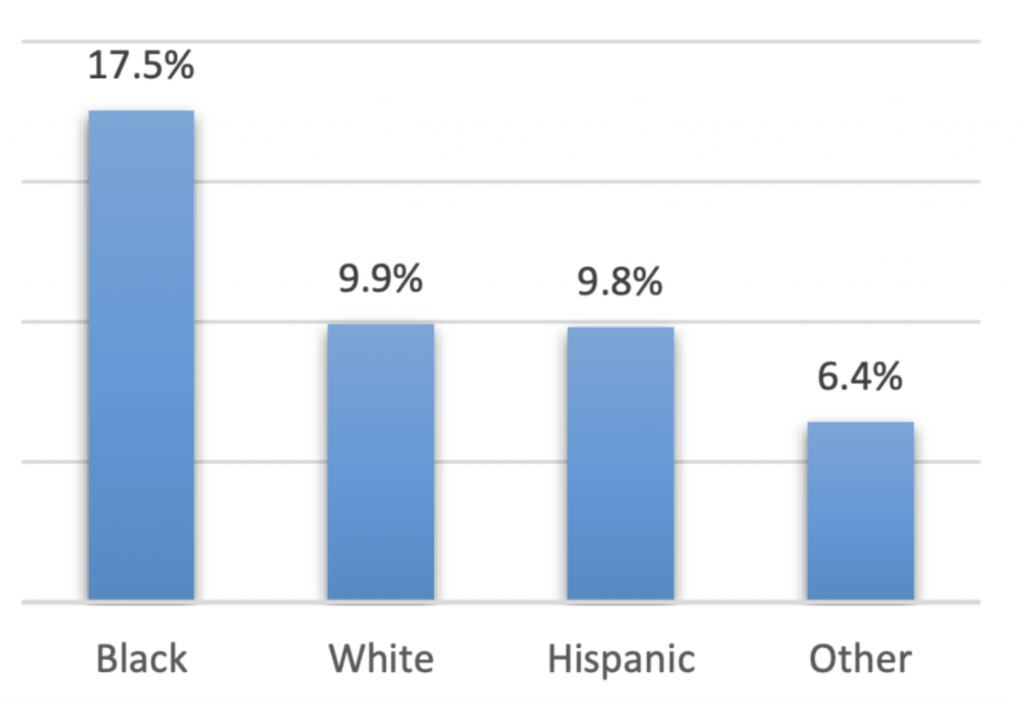
Increases in rates of diabetes, obesity and other related chronic diseases pose daunting challenges to Richmond public health. Nationally, 2021 was the second consecutive year in which more than 100,000 Americans died from diabetes (Chad Terhune and Robin Respaut, 2022). In Virginia, diabetes prevalence has continued to steadily rise over the last few years to a high of 11.1% as of 2020 (see figure 1). This statistic is slightly higher than the national value, 10.6%, and Virginia ranks 29th place in the race for healthiest state diabetes-wise (America’s Health Rankings, 2021). As a whole, the United States has a diabetes prevalence rate of African Americans in particular have disproportionately high-risk levels for diabetes and similar health outcomes such as high blood pressure, nearly doubling that of the second most at risk group, whites (17.5% to 9.9%, respectively) (see figure 2). These alarming statistics underscore the severity of yet another pandemic that rages among us: health equity and disparity.
Several studies have been conducted in which it was found that health is unevenly distributed across the socioeconomic spectrum: those of lower income, education, job status experience on average worse health and lower life expectancy than their counterparts with higher income or social standing (Nicole Lurie and Tamara Dubowitz, 2007; Eileen Crimmins, Samuel Preston, Barney Cohen, 2011; David Williams, 2006). More than that however, they also found that in neighborhoods with increasingly greater access to fast food restaurants, there were also greater percentages of unemployment and poverty (Michele Ver Ploeg, Vince Breneman, Tracey Farrigan, 2009). The reasons for this seem obvious: low-income residents live in worse environments, have less access to quality healthcare, and tend to eat more fast food. However, when taking a closer look at the food aspect of this issue, we find that there is more to this than fast food simply being convenient. Food security and accessibility, especially food deserts, are issues that require a closer analysis to understand and alleviate the role they play in perpetuating health inequity (National Research Council, 2009).
Food deserts are defined as “[areas] in the United States with limited access to affordable and nutritious food, particularly such [areas] composed of predominantly lower income neighborhoods and communities” in Congress’ 2008 Farm Bill (Angela Liese, James Hibbert, Xiaoguang Ma, et al., 2014). “Limited access” is measured by distance to the nearest supermarket “walkable” distances from those sources of food, as vehicle access and mobility often play important roles in people’s dietary choices. More specifically, “food deserts” refers to areas with no grocery stores within one mile in urban regions and within 10 miles in rural communities (Paula Dutko, Tracey Farrigan, Michele Ver Ploeg, 2012).
Food deserts are often found in low-income urban areas. Because one’s local food environment is so inextricably linked to their dietary patterns and health outcomes, unhealthy eating habits that stem from food deserts are linked to numerous acute and chronic health problems such as diabetes, hypertension, obesity, heart disease, and stroke (Heval Kelli, Muhammad Hammadah, Hina Ahmed, et al., 2017). Studies show that neighborhoods comprising mostly African Americans are more likely to be food deserts, as they often have lower access to supermarkets and other healthy food stores (Angela Hilmers, David Hilmers, Jayna Dave, 2012). A “food swamp” is an area where fast food locations greatly outnumber the healthy alternatives, and low-income minorities are more likely to live near/in these (Hilmers, Hilmers, Dave, 2012). These also have the adverse effect of shaping the food culture and habits of those residents into preferring fast food, something that holds much more weight in one’s dietary patterns than simply the proximity of a supermarket to their home.
Food Deserts in Virginia
In the wake of the 2008 Farm Bill and its discussion on food deserts, the food desert issue ascended to national prominence. In 2011, then-mayor of Richmond Dwight C. Jones strived to improve the health of city residents by addressing disparities affecting access to health care and resources by forming a “Food Policy Task Force” in which the results were published in 2013 (Matthew Becker, 2018). In it, it was found that food deserts were a major problem in the city, especially in the disadvantaged neighborhoods throughout Richmond City’s north side, south side, and east end (Becker, 2018).
Virginia shares in the aforementioned public health concerns, so it is to be expected that the state and its urban areas are no different. Studies on health equity in Richmond City, Virginia, have found that although African American residents comprise the predominant race in Richmond City (46.1% in 2021), they have often been segregated into the poorest neighborhoods in part due to historically discriminatory zoning policies (Emily Zimmerman, Amber Haley, Albert Walker, et al., 2016). In the past, highway construction and public housing projects worked in tandem with the socioeconomic conditions of African Americans to isolate their neighborhoods and prevent them from moving to suburban areas (Allison Shertzer, Tate Twinam, Randall Walsh, 2022). Because of the inescapable bond between poverty and the food environment, African Americans have a historically rooted increased risk of developing several preventable diseases such as diabetes (Hana Ames, 2021).
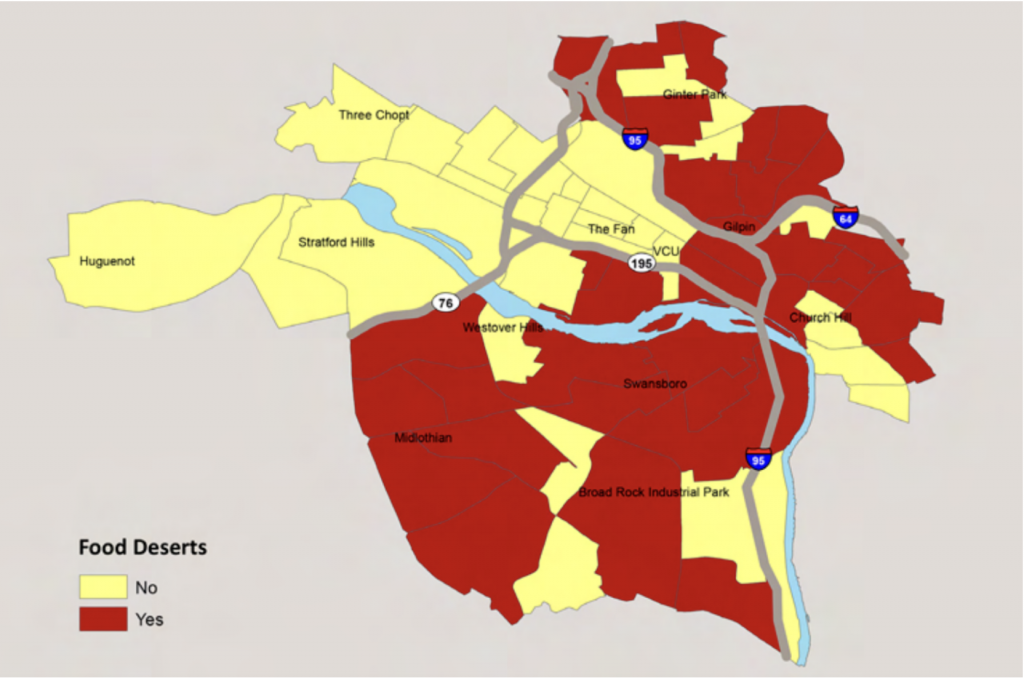
Additionally, like other mid-size cities, Richmond City’s income gap is already large but continues to grow. As of 2021, the Census Bureau estimated the percentage of Richmond City’s population in poverty to be 20.9% (U.S. Census Bureau, 2021). In 2016, the household income stood at just over $10,000 per year in the poorest census tract but was more than $175,000 per year in the wealthiest (Zimmerman, Haley, Walker, et al., 2016). This has made it so that life expectancy varies by 20 years for both genders combined across census tracts in Richmond City (Zimmerman, Haley, Walker, et al., 2016). In 2010, 56 tracts in metropolitan Richmond qualified as food deserts, with most of these tracts being in Richmond City (see figure 3). An estimated one million Virginians live in food deserts as classified by the previously mentioned definitions (Richmond Times-Dispatch, 2019), but it is prudent to remember that although many suburbs in Greater Richmond are classified as food deserts based on distance from supermarkets, because residents living in suburbs have much higher rates of vehicle access than their urban-dwelling counterparts, they can drive to a variety of supermarkets and have a wider array of food choices. However, many of the poorest neighborhoods in Greater Richmond tend to be poor suburbs on the outskirts of the city due to the houses being cheaper.
Food deserts have been identified as a serious issue in Richmond and addressing them is an important part of addressing certain health outcomes and building greater equity. This paper identifies current and past initiatives addressing food deserts in Richmond with the greatest potential for impacting sustainable health equity, considers the possible benefits as well as the likely limitations of these, and explores other strategies that might be undertaken.
Richmond’s Current Supermarket Scene
At first glance, Richmond seems like a well-off area in terms of supermarkets, and an inherent food inequity may not be obvious. In fact, in 2019 an article was written calling the Greater Richmond area “secretly the Supermarket Capital of America” (David Landsel, 2019). In a 2015 study done by Wallethub, Richmond was identified as 3rd place out of the 180 biggest cities in the US for most grocery stores per capita; 122.56 grocery retailers per 100,000 residents (Karri Peifer, Randy Hallman, 2015). In the same annual study in 2021, Richmond’s rank dropped, but still stood at a respectable 36th out of 180 for diversity, accessibility & quality of food (Adam McCann, 2021).
However, when taking a closer look at data provided by the Richmond government on the “grocery stores” in Richmond, it is clear that many of these “grocery stores” are in fact simply stores that sell food, such as convenience stores, gas stations, or Dollar Trees (Cara Davis, 2021). For example, the only “grocery store” listed in one of Richmond’s lowest median home value neighborhoods, on the outskirts of the city, Cofer, is EZ Mart, better known as Hopkins Store, a convenience store that sports only one small mini refrigerator with fresh fruit and vegetables thanks to the Healthy Corner Store Initiative (Richmond City GIS Hub, 2021). Likewise, Broad Rock is another low-income Richmond neighborhood touching Cofer in which the two “grocery stores” listed in the data are Your Neighborhood Convenient Store and Sea Farm, a combination fish market and seafood restaurant well known for its cheap fried oyster sandwiches and crab cakes.
These two Richmond neighborhoods not only lack a quality supermarket, but have a population composed of three fourths African Americans (Niche, 2022; Niche, 2022). Additionally, these are not the only neighborhoods in Richmond that follow this pattern. The connection between poverty and race may not be surprising, but the entangled connection between race, income, and the fulfillment of a basic need are alarming. In 2016, the Richmond Food Policy Task Force listed various recommendations such as further supporting the Healthy Corner Store Initiative, other community establishments and organizations, and incentivizing farmers’ markets and grocery stores as ways to address food deserts (Institute for Public Health Innovation, 2016). These recommendations will be evaluated below.
Healthy Corner Store Initiative
One of the principal initiatives targeting food deserts in Richmond that was implemented is the Healthy Corner Store Initiative, modeled after Philadelphia’s successful Healthy Corner Store initiative (Tammie Smith, 2015). The goals of this initiative established in 2012 consist of improving access to fresh produce at corner stores in USDA-recognized food deserts and low access neighborhoods, expanding exposure to and knowledge of fresh produce and nutrition through education and outreach events, and creating a viable farm-to-community hub model to make buying fresh produce cheaper and more sustainable (Smith, 2015). They do this by installing refrigerators covered by the non-profit in corner stores and partnering with Shalom Farms to allow store owners to buy the locally grown fruits and vegetables at prices lower than the wholesale cost. The corner stores can then offer it to customers for prices that are comparable or cheaper than they would find in a supermarket. From its USDA grant in 2017 to the termination of the grant in 2020, RHCSI was able to expand to serving 19 corner stores (U.S. Department of Agriculture, 2020).
Although RHCSI has grown a lot in the past decade and has had many beneficial impacts, there have also been many challenges to match these strides, particularly pertaining to its long- term goals. The first challenge has been creating a long-term model for corner stores to partner with local distributors to continuously offer fresh produce on their shelves. Because local distributors and corner stores could not agree on pricing that was financially viable for all the stakeholders in the matter, the primary distributor and producer for the program continues to be non-profit Shalom Farms (U.S. Department of Agriculture, 2020). Although this works fine for this specific program itself, this highlights a bigger issue that projects and initiatives such as this one face. Equity and profitability do not always overlap and offering fresh produce in a store in which the entire purpose is to sell cheap, quick food can be difficult to sustain, for both the store and a for-profit producer.
Often, many people traverse to corner stores specifically to buy cheap fast food in five minutes or less so the fact that there is fresh produce in the store does not hold too much significance. This is paired with the fact that there are other ingredients that one must buy to make dishes using fresh produce, and these other ingredients may not be offered at the corner stores. In the grant report for RHCSI, it was stated that “families were traveling the further distance in order to purchase produce at a conventional grocery store where all products could be purchased in one trip,” indicating that the intention of the trip to the store outweighed the geographical hurdles (U.S. Department of Agriculture, 2020). In addition to this, buying fresh produce means that the customer must not only have time to prepare that produce, but also the knowledge of what to do with it.
This issue also presents in fulfilling RHCSI’s other goal of providing food engagement and education opportunities such as cooking demonstrations and nutrition education with the community. Due to the in-and-out, fast-paced nature of corner stores, the events that they offered had low participation. Although the fruits and vegetables do sell in these corner stores, in fact selling out in many of the stores (Smith, 2015), the situation is reminiscent of fast-food restaurants offering salads: people will buy the salads, but people do not go to fast food stores specifically to eat salads, so is the offering doing anything substantial other than diluting food swamps?
The challenges that this initiative has faced spotlights a glaring issue that public health and food equity initiatives face on a larger spectrum: on what scale should food inequity programs be operating to focus on fixing the problem? Is the key to perpetuating supermarket and food equity through offering fresh produce in corner stores, or is this only a slight mitigation to the problem?
Community Gardens
Tackling food deserts from a different, community-oriented socio-cultural standpoint are various projects which aim to set up community gardens. Tricycle Urban Ag, formerly known as Tricycle Gardens, was a half-acre urban farm located in South Richmond, and as one of Healthy Corner Store Initiative’s partners, it promoted education on farming, soil improvement, and nutrition while also producing over 20,000 pounds of produce (Community Wealth, 2022). It began in 2010 and educated both adults and youth in the community on food and spearheaded the birth of community gardens and farms all around the city in efforts to increase healthy food access (Cause IQ, 2019). Unfortunately, in February of 2020, Tricycle had to shut down due to financial constraints stemming from a singular certification program that they had been holding (Smith, 2015).
Projects and organizations such as Tricycle Gardens are prime examples of targeting food insecurity and health inequity on a larger scope. They focus on the problems in lower-income communities that underlie health inequity such as lack of education and cultural habits of consuming unhealthy food. However, the fact stands that this decade old non-profit organization was proved financially unsustainable after a single program, even with $200,000 dollars in aid from the federal government and more than $300,000 in net lifetime assets (Mark Robinson, 2020).
Grocery Stores
When considering how fast money drains out of not-for-profit projects dedicated to minimizing food deserts such as Tricycle Urban Ag, it seems pertinent that a healthy medium between Tricycle Urban Ag and the Healthy Corner Store Initiative is established in order to effectively target the roots of food deserts. One solution that could be proposed is building more supermarkets or creating incentives and assistance for new grocery store developments in food deserts. However, there has been fear expressed that these incentives could precipitate potential gentrification by causing wealthier people to move into the poorer neighborhoods (Caitlin Morris, 2019).
Going hand in hand with this concern is the fear that development in disadvantaged communities could lead to higher rents and the loss of small businesses. These misgivings helped to kill Virginia Senator Warner’s Healthy Food Access for All Americans Act in Congress in 2021, which proposed to provide tax credits and grants to grocery stores, food banks and other organizations that provide healthy foods in underserved communities (117th Congress, 2021). The difficulty of passing bills targeting food deserts and incentivizing the development of supermarkets, in addition to the slow-moving pace of legislation passage and the concerns about gentrification, culminate in this potential solution being an unsatisfactory short term one. One benefit of supermarkets, however, is that they offer many ready-to-go meals in addition to fresh produce. Convenience plays a huge factor in low-income households’ meal choices, and being able to buy fresh meals that require no preparation is very valuable.
Farmers’ Markets
Ready-to-go meals are also a fixture at farmers’ markets, which make them an attractive option for a potential alleviation of the food desert issue. Farmers’ markets are public and recurring assemblies of farmers in which farmers sell produce directly to their consumers, including those that receive food assistance (Andrea Brace, Todd Moore, Todd Matthews, 2020). These assemblies also facilitate personal connections and bonds of mutual benefits between farmers, customers, and communities, which may help the food culture setback that low-income individuals face. In addition to this, farmers markets can also provide nutritional information on food, just as Tricycle Gardens did and just as the Corner Store Initiative has had trouble with.
Farmers’ markets are also cheaper to implement than entire new supermarkets. The USDA noted that farmers’ markets are “less expensive [to implement], require less space, and can be quicker to implement than programs that encourage new store development”, and thus recommend it as a community-level intervention for food deserts (Brace, Moore, Moore, 2020). One setback of farmers’ markets is that weather and season are often a factor in administering farmers’ markets. However, markets can also be located indoors and there is constantly fresh produce in different seasons. With a strong partnership between the market and the community, sufficient connections with and assistance from government programs and well thought out site selections, farmers’ markets could be a very big asset to the Richmond fight against food deserts.
Conclusion
Food deserts and the health outcomes linked to them, such as diabetes, are huge problems in Richmond, VA. Although there have been many proposed solutions and solutions that have been enacted, not all of them are equally effective. The most effective solution that could be implemented quickly and readily is establishing farmers’ markets in various underserved and low-income areas in Richmond. Richmond City could grant money for this purpose, and a small team of dedicated people to staff these farmers’ markets could help this run smoothly.
Long-term wise, supermarkets being built in these areas would probably be the best solution to alleviating food deserts. Because legislation that would shore up funds and the framework for incentivizing the building of these supermarkets takes so long to pass, this is something that would have to be worked on while farmers’ markets temporarily allay the need for a healthy food environment alone along with initiatives like the Healthy Corner Store Initiative. Because supermarkets and farmers’ markets offer fresh produce and fresh ready-to-eat meals that play a big factor in low-income individuals’ choices for food, especially households, these are the most viable solutions. Additionally, the ease of being able to incorporate EBT and SNAP, food assistance programs, into supermarkets and farmers’ markets is also useful. Price manipulation, such as increasing prices of unhealthy foods to subsidize lowering the costs of healthy foods, and/or offering coupons and other incentives at these stores to buy healthier food could also be considered as a mechanism to promote healthier eating.
Regarding concerns about gentrification occurring with both supermarkets and farmers’ markets, this could possibly be diminished by offering incentives and/or benefits for locals to shop at those stores. Additionally, it is valuable to understand that gentrification may hold some potential benefits because although the price of property rises, the quality of life also rises. Steps can be taken to prevent pushing poorer people out even with economic progress in the community. However, that is a topic beyond the food scene.
Appendix
Figure 1
Diabetes Prevalence in Virginia
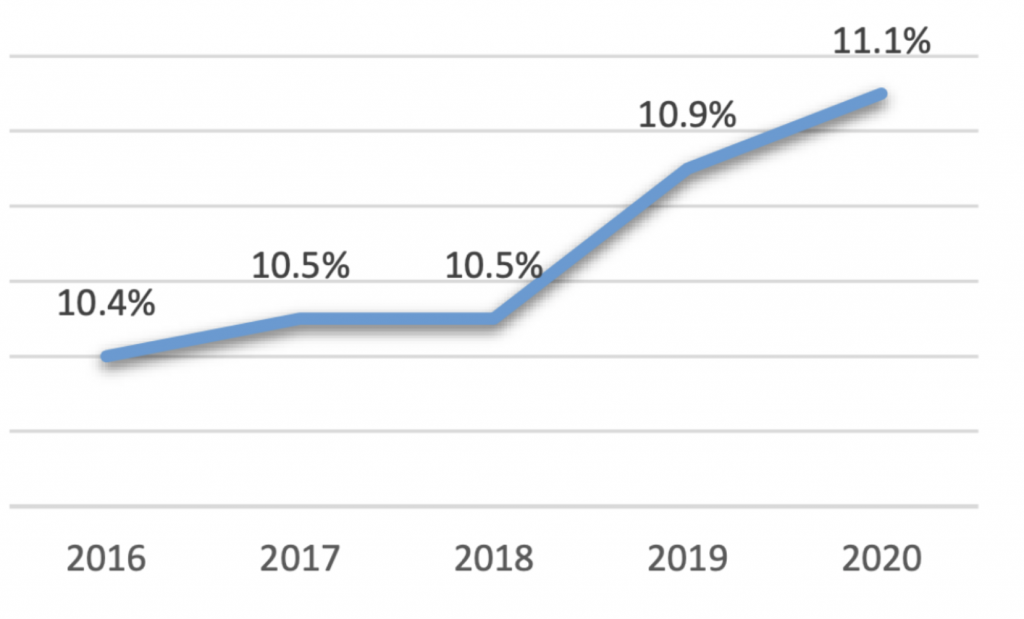
Figure 2
Prevalence of Diabetes in Virginia by Race/Ethnicity in 2019
Microsoft Word – Joanne Lin Mentorship Paper.doc
Figure 3
Census Tracts Qualifying as Food Deserts, Richmond City, 2020
References
Ames, H. (2021, March 29). Why is diabetes more common in African Americans? Medical News Today. https://www.medicalnewstoday.com/articles/diabetes-in-african- americans#males-vs-females
Becker, M. (2018, May). Implementation Plan for the Maggie Walker Community Land Trust to Operate as a Land Bank. Virginia Commonwealth University. https://scholarscompass.vcu.edu/murp_capstone/6/
Brace, A., Moore, T., & Matthews, T. (2020). The Relationship Between Food Deserts, Farmers’ Markets, and Food Assistance Programs in Hawai’i Census Tracts. Hawai’i Journal of Health and Social Welfare, 79(2). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7007308/
Broad Rock. (n.d.). Niche. https://www.niche.com/places-to-live/n/broad-rock-richmond- va/#residents
Burns, J. (2015, March 3). ‘Living in a Food Desert’ looks at a problem you may not know about. WTVR-TV. https://www.wtvr.com/2015/03/03/living-in-a-food-desert-looks-at-a- problem-you-may-not-know- about/#:~:text=Last%20year%2C%20a%20group%20of,as%20one%20too%2C%20resea rchers%20said.
Cofer. (n.d.). Niche. https://www.niche.com/places-to-live/n/cofer-richmond-va/#residents
Crimmins, E. M., Preston, S. H., & Cohen, B. (2011). Explaining divergent levels of longevity in high-Income countries. National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK62362/
Davis, C. (2021, May 14). Combating Food Deserts in Richmond, VA:. https://storymaps.arcgis.com/stories/a9c13d04f3ed440ca7011ad297514479
Diabetes in the U.S. (2021). America’s Health Rankings. https://www.americashealthrankings.org/explore/annual/measure/Diabetes
Editorial: No Food Deserts. (2019, March 14). Richmond Times-Dispatch. https://richmond.com/opinion/our-opinion/editorial-no-food-deserts/article_ddf9d697-ced7-57f0-93b5-e658bcc999b0.html
Ferm, J. (2016). Preventing the displacement of small businesses through commercial gentrification: Are affordable workspace policies the solution? Planning Practice & Research, 31(4), 402-419. https://doi.org/10.1080/02697459.2016.1198546
Grocery Stores: Richmond, Virginia. (2021). Richmond City GIS Hub. https://docs.google.com/spreadsheets/d/e/2PACX- 1vQj6DRKARByNqOTwMDNDZPLRcP8Nyc1P0avH8Egag8eszBSsmofm4Na_M3jRN KStRpn6G_vPSFb8eJh/pubhtml?gid=1774930533&single=true&widget=true&headers=f alse
Healthy Food Access for All Americans Act, S. 203, 117th Cong. (as referred to Senate Committee, Feb. 3, 2021). https://www.congress.gov/bill/117th-congress/senate- bill/203/actions?q=%7B%22search%22%3A%5B%22s.+203%22%5D%7D&r=1&s=5
Hilmers, A., Hilmers, D. C., & Dave, J. (2012). Neighborhood disparities in access to healthy foods and their effects on environmental justice. American Journal of Public Health, 102(9), 1644-1654. https://doi.org/10.2105/AJPH.2012.300865
Kelli, H. M., Hammadah, M., Ahmed, H., Ko, Y.-A., Topel, M., Samman-tahhan, A., Awad, M., Patel, K., Mohammed, K., Sperling, L. S., Pemu, P., Vaccarino, V., Lewis, T., Taylor, H., Martin, G., Gibbons, G. H., & Quyyumi, A. A. (2017). Association between living in food deserts and cardiovascular risk. Circulation: Cardiovascular Quality and Outcomes, 10(9). https://doi.org/10.1161/CIRCOUTCOMES.116.003532
Lacey, A. (2017, June). The Corner Store Initiative is Positively Richmond. WRIC-TV. https://www.wric.com/news/the-corner-store-initiative-is-positively-richmond/
Landsel, D. (2019, January 9). This City Is Secretly The Supermarket Capital of America. Food & Wine. https://www.foodandwine.com/news/best-supermarket-city-in-america
Liese, A. D., Hibbert, J. D., Ma, X., Bell, B. A., & Battersby, S. E. (2014). Where are the food deserts? An evaluation of policy-relevant measures of community food access in south carolina. Journal of Hunger & Environmental Nutrition, 9(1), 16-32. https://dx.doi.org/10.1080%2F19320248.2013.873009
McCann, A. (2021, October 4). Best Foodie Cities in America. WalletHub. https://wallethub.com/edu/best-foodie-cities/7522
Morris, C. (2019, April 2). How to attract grocery stores to Richmond’s ‘food deserts’. WTVR- TV. https://www.wtvr.com/2019/04/02/richmonds-food-deserts
Peifer, K., & Hallman, R. (2015, October 14). Survey: Richmond ranks near top in number of grocery stores per capita. Richmond Times-Dispatch. https://richmond.com/food- drink/survey-richmond-ranks-near-top-in-number-of-grocery-stores-per- capita/article_4dca25ea-7283-11e5-af9f-573ee0494952.html#:~:text=The%20grocery- stores%20statistic%20was,categories%20in%20WalletHub%27s%20weighted%20formu la
Richmond City Food Policy Analysis and Recommendations — A Report to the Richmond Food Access and Equity Task Force. (2016, October). Institute for Public Health Innovation. http://www.institutephi.org/wp-content/uploads/2017/02/Richmond-City-Food-Policy- Recommendations-Report-FINAL.pdf
Richmond City, Virginia QuickFacts. (2021). United States Census Bureau. https://www.census.gov/quickfacts/richmondcityvirginia
Richmond Healthy Corner Store Initiative Expansion Project. (2020). United States Department of Agriculture. https://portal.nifa.usda.gov/web/crisprojectpages/1013245-richmond- healthy-corner-store-initiative-expansion-project.html
Robinson, M. (2020, February 28). Tricycle Urban Ag, Church Hill-based nonprofit, transferring property, ceasing operations. Richmond Times-Dispatch. https://richmond.com/news/local/tricycle-urban-ag-church-hill-based-nonprofit- transferring-property-ceasing-operations/article_997ee77e-ccb1-587a-804f- 0c06b306097b.html#:~:text=Chief%20Jason%20Weller%20of%20the,Bainbridge%20Str eet%20in%20South%20Richmond
Shertzer, A., Twinam, T., & Walsh, R. P. (2022). Zoning and segregation in urban economic history. Regional Science and Urban Economics, 94, 103652. https://doi.org/10.1016/j.regsciurbeco.2021.103652
Smith, J. P. (2007). The impact of socioeconomic status on health over the life-course. Journal of Human Resources, XLII(4), 739-764. https://doi.org/10.3368/jhr.XLII.4.739
Smith, T. (2015, June). Your Health: Healthy Corner Store Initiative. Richmond Times-Dispatch. https://richmond.com/your-health-healthy-corner-store-initiative/article_c1b86490-d018-5aa7-8d0a-beb491230191.html
Terhune, C., & Respaut, R. (2022, January 31). Exclusive: U.S. diabetes deaths top 100,000 for second straight year. Reuters. https://www.reuters.com/world/us/exclusive-us-diabetes-deaths-top-100000-second-straight-year-federal-panel-urges-2022-01-31/
Tricycle Gardens. (n.d.). Community Wealth. https://community-wealth.org/content/tricycle-gardens
Tricycle Gardens. (2019). Cause IQ. https://www.causeiq.com/organizations/tricycle-gardens,753253795/
United States Department of Agriculture. (2009, June). Access to Affordable and Nutritious Food-Measuring and Understanding Food Deserts and Their Consequences: Report to Congress (M. Ver Ploeg, V. Breneman, & T. Farrigan, Authors).
United States Department of Agriculture. (2012, August). Characteristics and Influential Factors of Food Deserts (P. Dutko, M. Ver Ploeg, & T. Farrigan, Authors). https://www.ers.usda.gov/publications/pub-details/?pubid=45017
Virginia diabetes data brief. (2021, June). Virginia Department of Health. https://www.vdh.virginia.gov/content/uploads/sites/25/2022/03/Diabetes-Data-Brief.pdf
Williams, D. R. (1999). Race, socioeconomic status, and health the added effects of racism and discrimination. Annals of the New York Academy of Sciences, 896(1), 173-188. https://doi.org/10.1111/j.1749-6632.1999.tb08114.x
Zimmerman, E., Haley, A., Walker, A., Woolf, S., Nguyen, K., Shue, W., Kelley, L., Hellman, J., & Chapman, D. (2016). Richmond Health Equity Report. Virginia Commonwealth University. https://societyhealth.vcu.edu/work/the-projects/richmond-health-equity- report.html
About the author
Joanne Lin
Joanne is currently a high schooler from the suburbs of Virginia. She loves science and history and plays volleyball and volunteers as an EMT outside of school. Joanne has won statewide awards for her historical documenting endeavors and she also works in research labs to satiate her interest in how the world works and how she can help it. Most of all, Joanne loves hanging with her family and friends and eating food from around the world!
