Author: Sana Gupta
Mentor: Dr. Emma Sarro
Pierre Elliott Trudeau High School
Abstract
COVID-19 virus has invaded the world, just like how cancer spreads from one body part to another and slowly invades our whole body. A virus is a very small particle that can cause an infection and has the ability to only replicate in its host cell. COVID-19, first identified in Wuhan, China, is a type of Coronavirus whose infection has caused the world’s deadliest pandemic. This infection is caused by the airborne virus named SARS-CoV 2 virus and can cause symptoms from mild cold and cough to serious respiratory problems. But the problems are not limited to physical health, it can extend to mental well-being as well. Many have suggested k that people might go into depression after contracting COVID-19 as a result of external factors like weakness, loneliness, a lack of social life, lower incomes etc. While these factors may be a part of the reason, what if the real root cause of this problem is the entry of the virus into the brain and manipulating its functioning? This review article will discuss this possibility. It will also discuss the possible mechanisms of the COVID-19 virus to enter the brain. For example- It could enter through the olfactory nerve, cribriform plate, or the Angiotensin converting enzyme 2 which is present in the blood brain barrier.
Introduction
The word ‘pandemic’ has been circulating in our mouths for quite some time now. We have been living under the rule of a virus named Coronavirus or more specifically COVID-19 for the past 2.5 years and these years have been difficult for everyone. This pandemic has shaken the world completely and things seem to be far from normal. Taking rapid antigen tests is a part of our daily routine now, and masks and face shields have become an accessory. Despite knowing the seriousness of this virus and its effects, people have started to take it lightly but have you ever wondered that once this pandemic ends, it still can have long term effects on us?
The COVID-19 pandemic is an ongoing global pandemic that is caused by severe acute respiratory syndrome coronavirus 2. This virus was first identified in Wuhan, China in December 2019. Unfortunately, this virus spread around the whole world and the World Health Organization declared it a pandemic on 11th March, 2020. As of August 1st, 2022, there have been more than 577 million cases and 6.4 million confirmed deaths and this makes it one of the deadliest pandemics in history. (Wikipedia, 2022)
This is an air-borne disease and transmission can also occur if contaminated fluids reach the eyes, mouth or nose. COVID-19 can be symptomatic as well as asymptomatic making it even more harmful and an infection to be extremely cautious of. Some of the symptoms that appear in infected patients are fever, headache, loss of taste and smell, sore throat, nausea, diarrhea and many more. COVID-19 virus not only affects physical health but also mental health, it has also been found that those infected are also suffering from mental disorders like depression and anxiety, due to which the cases of depression and anxiety have skyrocketed ever since the pandemic. In fact, it has been found that among more than 3900 people who contracted COVID-19 between May 2020 to January 2021, 52% of them showed signs of depression. One in five COVID survivors develop mental disorders like depression, anxiety or dementia. A survey funded by the Alberta Charitable Health Foundations found that 50% of the 6000 people that were surveyed had anxiety, 40% were depressed and about 85% had moderate to high stress. Symptoms under the umbrella of anxiety and depression that have been reported alongside the pandemic are excessive nervousness, fear, worry, lack of energy, and agitation. These symptoms suggest that the external factors of the pandemic (loss of job, fear of contracting the virus etc) may be responsible for the upswing in depression and anxiety, however, it is also possible that the virus itself may be able to enter the brain, directly causing the above mentioned symptoms. (Weber, 2020; Government of Canada, 2021; WebMD, 2022)
This paper will address the question of whether a virus, such as the current COVID-19, could directly impact how we feel, or our mental state. We will first discuss the different ways that other known viruses have been known to either have direct or indirect access to the brain and what mechanisms we propose they have used.
Viruses with indirect access
From what we currently understand, there are both indirect and direct ways that a virus can impact brain function and human behavior. Here we will cover several examples of viruses, one of which can have both direct and indirect access, and one that only can access indirectly. Influenza is a viral infection that attacks and deteriorates your respiratory system which includes lungs, throat and nose. Influenza can attack any age group and its symptoms include fever, headache, chills, muscle aches, persistent cough, ear pain etc. Influenza patients also show symptoms of anxiety and depression and studies have found that it is said to have an indirect relation with anxiety, depression and PTSD. If a patient is under stress, or anxious or depressed then his/ her immune responses to the Influenza vaccines reduces drastically. The reason behind this is that when a person is anxious or depressed or is going through mental health issues then there are changes in the neuroimmune pathways which causes stress related immune disregulation which decreases the body’s influenza antibodies’ response to the virus and hence influenza can be more serious in patients who have anxiety or depression. Studies and surveys are being conducted to find a deeper relation between influenza and depression and anxiety. However, studies have shown that state anxiety which is a temporary emotional condition followed by tension and fear of a particular event or activity has positive effects with Influenza antibodies. Such people tend to take extra personal hygiene care because they have the fear of the pandemic. Similarly, when people with ARDS (intensive for the influenza infection) are admitted in ICU, they are likely to develop PTSD. Interestingly, despite so many studies showing evidence for indirect linkages through neuroimmune pathways to the neurological diseases and effects, Influenza has shown to have a direct connection with one neurological disorder which is the stroke. The seasonal variation in stroke has been related to respiratory tract and influenza infections. Patients with increased respiratory tract infections are more susceptible to stroke. Influenza virus can cause stroke through the inflammatory mechanism. During the infection, the respiratory tract releases cytokines into the blood that induced macrophage inflammatory protein-2 and other inflammatory mediators in the ischemic brain. This is followed by disruption of the blood brain barrier which causes an increased rate of intracerebral hemorrhages after tissue plasminogen activator treatment. Stroke is generally caused by a pre-existing state of inflammation due to atherosclerosis, obesity, or infection. The systemic inflammation due to lipopolysaccharides may aggravate neuroinflammation in cerebral ischemia and thus cause a stroke. Studies are being conducted to provide deeper evidence and connection of the systemic inflammation (neural inflammation) with the influenza virus. (Coughlin, 2012; Mayo Clinic, 2021; Mohammad,2011)
HIV (Human Immunodeficiency Disease) is a retrovirus that can cause a breakdown of the body’s immune system. Contracting HIV virus can lead to the development of AIDS (Acquired Immunodeficiency Syndrome). This syndrome marks the array of diseases and malignancies and is diagnosed by the presence of T cells, cancer and opportunistic infections. It can be transmitted through blood, sexual contact or perinantal care. HIV has a very interesting indirect mechanism related to neural disorders. Although neurodegenerative disorders like depression, PTSD, stress may develop after contracting HIV, the reverse can also take place. People who are diagnosed with PTSD, stress related disorders or depression are more likely to engage in sexual activities, drug and alcohol use and as a result be exposed to the virus and develop AIDS. Evidence from various surveys also proves that patients with depression, PTSD were diagnosed with HIV/AIDS as well. Patients with PTSD had advanced symptoms of HIV, prior history of trauma and greater perception of stigma. Patients with HIV may develop depression as a result of disease progression. Some antiretroviral treatment may cause the CNS to be toxic and depression and disruption of sleep may develop as result of the treatment. Further studies are being done to find a more detailed link between HIV/AIDS and neurodegenerative disorders. (NASW, 2019; Coughlin, 2012)
Viruses with direct access
There are a few viruses that seem to have direct access to the brain. For example, Herpes simplex encephalitis is a contagious infection caused by the herpes simplex virus which is a neurotropic double stranded DNA. Its symptoms include fever, headache, nausea, fluid-filled blisters etc. This infection impacts the temporal and frontal lobes of the brain which leads to edema, hemorrhage and necrotic changes in the brain parenchyma. It has been found that the herpes infection has a direct connection with neurodegenerative disorders. In some hosts, this virus may produce changes in the cellular processes that are required for the normal function of the neurons. Followed by the infection, there are changes in the permeability of the blood brain barrier because of which it is easy for the virus to disrupt the blood brain barrier and infect the brain parenchyma and this increases the movement of the virus, cytokines and the immune cells into the brain. Since the immune system responds as soon as the virus enters, the immune cells that enter the Central Nervous System to disrupt the virus may be responsible for the chronic inflammation of the brain tissue which can give rise to disorders like stroke, Alzhemiers etc. Moreover, it has been found that stress, depression and anxiety are also related to the infection caused by the virus. Stress and psychological disorders can result in shingles in people who are not vaccinated. Lastly, depression decreases the vaccination’s immunity response to the virus due to which the effect of the virus can increase in depressive people. As one starts aging, there is a decrease in the immune response to the zoster vaccine due to which the virus may activate again (if they were infected earlier) or can easily enter the organism’s body. (Coughlin, 2012; Liu, 2018; Duarte, 2019)
Hepatitis is a viral infection that causes the inflammation of the liver. It can be caused by three types of viruses namely- Hepatitis A, Hepatitis B and Hepatitis C. The liver is an important part of our body, it helps in performing numerous functions like filtering of the blood, processing nutrients and fighting infections. If the liver is damaged, then all the other organs would be adversely affected. Depression, fatigue and neurocognitive deficits are the major symptoms of this disease. The mechanism of the virus to get into the brain is similar to the way the herpes virus enters the brain. The hepatitis virus too disrupts the blood brain barrier which increases the exposure of the CNS to the virus, cytokines and the immune cells which in turn inflates the tissues of the brain. These intracerebral changes lead to the symptoms of the infection which are depression and neurocognitive diseases. HCV ribonucleic acid has been found in the peripheral blood mononuclear cells, cerebrospinal fluid and the brain of chronically infected patients. Additionally, depression may lead to increase in psychological stress, and physical symptoms of the disease. (CDC, 2020; Coughlin, 2012; Yeoh, 2018; Stanculete, 2017)
Given the above information, it’s possible that the Sars-CoV virus has direct access to the brain and could directly cause the symptoms, like Herpes and Hepatitis. This paper will present the evidence above as well as several recent studies around the mechanisms of Corona viruses and those similar to answer this question.
Methods
For this article, research was done by reading through and extracting information from many articles. The main search engines used to collect research articles were Google Scholar and Wikipedia for other information around the viruses. Our research included data and statistics from 2018. The main keywords used while researching were depression, anxiety, COVID-19, SARS, age based groups, mechanisms of the entry point of the virus, angiotensin converting enzyme 2, names of various viruses like Influenza, Hepatitis C, Herpes and HIV. Our study mostly included studies that examined individuals from all age groups except for connection between COVID-19, depression and age based groups which included people from 18 to 40 years of age. This paper primarily talks about effects and mechanisms of COVID-19 and SARS into the brain in a human body except for the entry point of SARS into the brain through the olfactory nerve which was for now tested in wild mice which was under the control of human cytokeratin 18 promoter. This review investigates if COVID-19 virus can enter the brain or not and cause neurological disorders like depression, anxiety, PTSD etc and its mechanism of entering the brain if it is possible. An important factor while searching the articles was to make sure to find the direct mechanism of the entry of COVID-19 into the brain rather than through entering other organs (ex-lungs) first.
Results
Points of entry and virus structure
Studies are showing that, it is possible that SARS-CoV, similar to MERS-CoV, infects the lungs and the brain, however, the timing of infecting the 2 organs is different. The virus attacks the brain much later than the lungs which shows that the virus follows a hematogenous route of infection which indirectly affects the functioning of the brain. Furthermore, SARS-CoV infected the vital brain stem nuclei in wild mice which was under the control of the human cytokeratin 18. There was no initial inflammation of the neuronal tissues but at day 4, signs of inflammation were seen. But did the COVID-19 virus enter the brain directly or indirectly and if it entered directly, what could be the possible mechanisms? (Natoli, 2020)
Below we cover several possible entry points for the virus given the work on it or similar viruses.
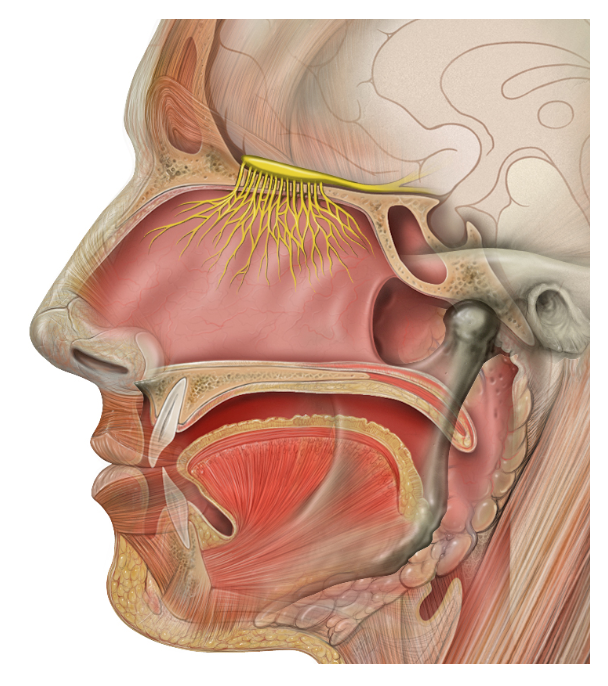
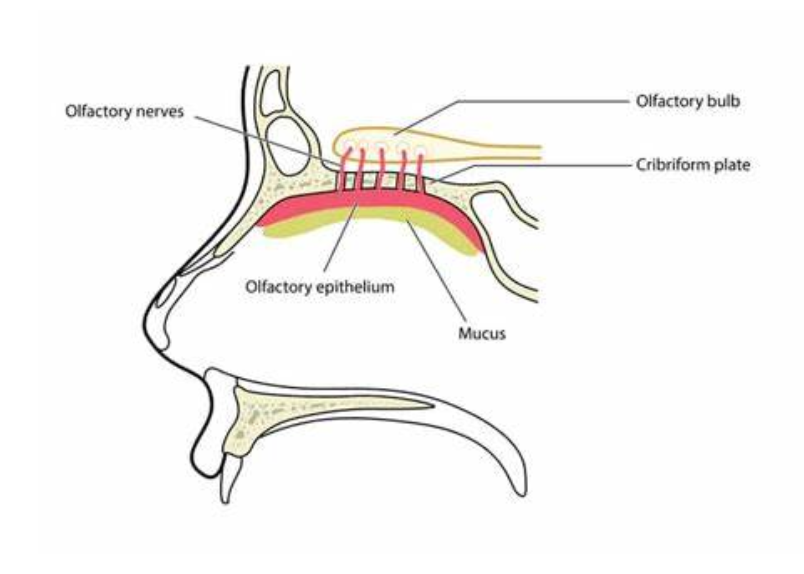
Olfactory nerve The olfactory nerve is one way through which the SARS CoV could get into the brain. The olfactory nerve is a cranial nerve that contains sensory nerve fibers relating to the sense of smell. The afferent nerve fibers are responsible for transmitting impulses about odors to the Central Nervous System. The yellow coloured fibers depicted in Figure 1 are the olfactory nerve fibers. Since the nose is one of the ways by which the virus can enter our body, so as soon as the virus enters through the nose, it can come in contact with the olfactory nerves since the olfactory nerves and nose are connected so the COVID-19 virus could get attached to any of the fibers of the olfactory nerve and it could easily enter the brain in no time. Moreover, it also explains the symptom of loss of smell when we are diagnosed with this infection. The most probable reason is because the virus affects the functioning of the olfactory nerve fibers due to which they cannot transmit the impulses of odor to the brain and hence we cannot smell anything. An experiment that was tested on wild mice which was under the control of the human cytokeratin 18 promoter showed that the virus infected the respiratory epithelium and then the alveoli, however, the kinetic profile of the viral antigen showed that the virus infected the olfactory bulb first and then gradually infected the subcortical and cortical regions thus showing that the virus infected the brain. (Natoli, 2020; Wikipedia,2022)
Enzyme activation through Blood Brain Barrier Although COVID-19 is suspected to have side effects on the respiratory system of an organism, studies have shown that it can have an effect on the brain too through various mechanisms. One such mechanism is the angiotensin converting enzyme 2 that is present in the blood brain barrier. The blood–brain barrier (BBB) is a physicochemical barrier that constrains the entry of molecules and toxic substances into the brain. It is composed of Blood endothelial cells that limit the entry of molecules with molecular weights higher than 500 Da into the brain. However, many infectious agents manipulate the machinery of the brain endothelial cells to gain access to the brain. As mentioned earlier, one such machinery is the Angiotensin converting enzyme 2 which can be found on the membranes of the cells in the intestines, kidneys, heart and gallbladder or can also be found in the soluble state. It can also be found in the cytoplasm of the cell bodies of the neurons. It is an important part of the renin angiotensin aldosterone system which is responsible to keep the body’s blood pressure normal. The CoV spike glycoprotein has a very high affinity for the angiotensin converting enzyme 2 (a major reason is due to the sluggish movement of blood in the brain due to which it can easily come in contact with the above mentioned enzyme) and immediately binds with it thereby causing changes and damage to the body’s blood pressure system. This will affect the normal functioning of molecular delivery into the brain which would be a major pathway for the virus to enter the brain. If the virus enters the brain, it would cause dysfunction of the brain and these metabolic changes in the brain can lead to various neurological disorders. As a result, there would be changes in the functioning of the mitochondria of the endothelial cells in the brain which would lead to higher chances of stroke. Lastly, post mortem reports of those infected have detected the SARS-CoV N protein and the RNA polymerase gene fragment in the neurons along with the angiotensin converting enzyme 2 in the neurons and the endothelial cells of the brain which suggests that SARS has an entry point into the brain through the angiotensin converting enzyme 2. (Natoli, 2020; Wikipedia, 2022; Kim, 2021)
Cribriform plate: The Cribriform plate is a sieve like, spongy structure between the anterior cranial fossa and the nasal cavity. It is a part of the ethmoid bone and its deep grooves support the olfactory bulb. Since this cribriform plate is sieve like and is connected to the nasal passage as well as the olfactory bulb, there is a possibility that when the COVID-19 virus enters our body through the nose, it passes through this cribriform plate where it has access to the olfactory bulb and in turn to the olfactory nerve. (Baig, 2020)
Age-related or demographic evidence
Have you ever wondered that some age groups might be more prone to the COVID-19 virus entering their brain than others? Have you thought that even though we have physically recovered from COVID-19, we can still suffer from its long-term effects? Specifically, some age groups might have less mortality rate than others but they surely have longer after effects.
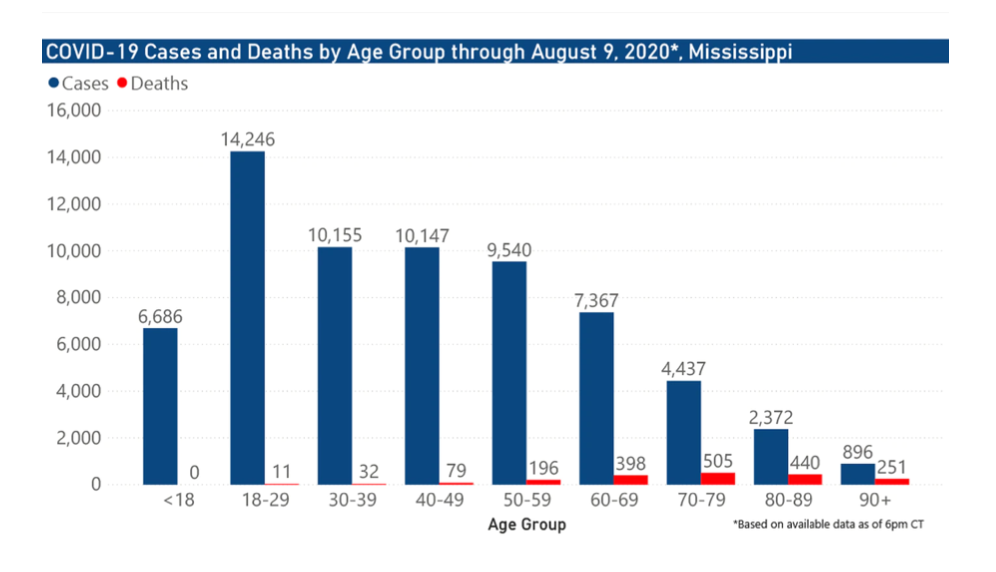
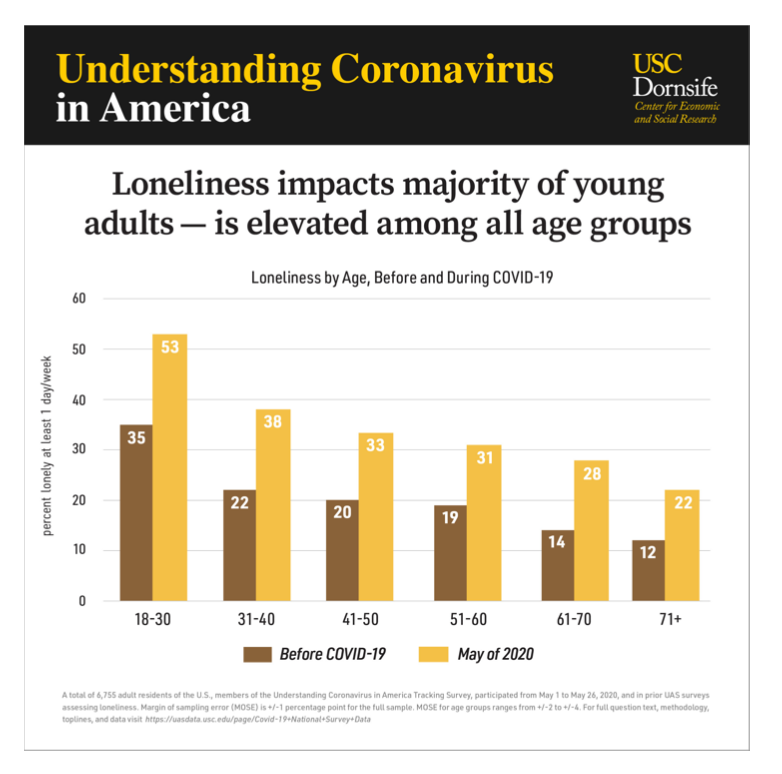
Young adults between 18-29 years of age are the most susceptible to suffering due to COVID-19 even though they have recovered from the infection. As shown in the Figure 3 and Figure 4, there were more than 14,000 cases just amongst 18-29 years of age making it the highest number of cases amongst all age groups and more than 50% of people between 18-29 years of age suffered from loneliness after the pandemic respectively. The probable reason behind this data is the physical maturity of the brain.
It has been found that the brain is underdeveloped at least till 25 years of age and is under the process of developing between 25-30 years of age. Different regions of the brain develop at different times. Significant changes in brain anatomy and activity take place during young adulthood, especially in prefrontal regions that are important for planning ahead, anticipating the future consequences of one’s decisions, controlling impulses, and comparing risk and reward. Hence, due to this if the virus enters the brain of an 18-29 old adult, then it can easily disrupt the barriers of the brain and dysfunction its cells because the brain is still developing, so the barriers of the brain cannot fully protect the brain since it is still achieving maturity. So, once the virus enters the brain. It can manipulate its functioning and its various regions and mechanisms due to which a person might feel lonely, depressed or anxious. Moreover, during depression, a person likes to detach themselves from their family and friends which increases their lonelinessThis proves the reason as to why adults between 18-29 years of age have increased rates of loneliness during the pandemic. (The New York Times, 2012)
Discussion
The pandemic indeed is very scary and dangerous for us in many ways, the majority of which causes harm to our physical and mental well-being. Everyone says that the virus has to mutate enough to die one day but little did they know that even though the virus is no longer alive, its effects are.
This study not only helped us gain information about the various mechanisms of COVID-19 virus into the brain but also about the effects of prevailing viruses, which we treat as normal, on the brain. It can be predicted that the mechanisms of the COVID-19 would be very similar to the prevailing viruses and hence, we can build upon those viruses to formulate various hypotheses for COVID-19 and how it can cause depression or anxiety. In some cases, depression or anxiety can worsen a person’s condition if he/she is infected with a virus. For example, in the case of HIV and Influenza, if a person is suffering from depression previously, and he/she is infected with HIV or Influenza, then depression would deteriorate a person’s condition even more because the immunity of the antibodies, that are supposed to defend the body by fighting against the virus, decreases. But, Influenza can infect the brain directly also through the inflammation of the neuronal tissues and thus enter the brain. In addition to Influenza, viruses like Hepatitis C and Herpes can damage the brain by disrupting the blood brain barrier, due to which the viruses come in contact with the Central Nervous System and cause dysfunctioning of the brain leading to depression, anxiety or other neurological disorders.
The main form of platform used for the above and following information was Google Scholar and all the statistics and data are collected after 2018. All the trials that are studied throughout this paper are mainly executed on humans or by using human kinematics in another organism.
Various studies and evidence have displayed the various mechanisms through which the COVID-19 virus could also enter the brain, disrupt its functioning and cause depression or anxiety. For instance- the virus could enter through the nose and come in contact with the olfactory nerves through which it can easily access the brain and its endothelial cells and damage the normal functioning of the brain. Another mechanism is through the blood brain barrier which contains the Angiotensin converting enzyme 2. COVID-19 virus has high affinity for this virus due to which it can easily bind with it and manipulate into a completely different function, thus interfering and disrupting the functioning of the brain.
Lastly, it is probable that there might be some correlation between the age of a person and number of cases of depression during the pandmeic. It has been found that the number of cases of COVID and loneliness between 18-29 years has tremendously increased during the pandemic. This can be related to the maturity of the brain. The brain does not develop until 30 years of age, until which the virus can easily attack the developing regions of the brain and enter. Like all the other viruses it would disrupt its functioning, thereby causing neurological disorders like depression which increases the rate of loneliness.
Clinicians and people must be cautious of this virus. Even though people have physically recovered from it, it would still impact their mental well-being because of which it is important to come in contact with the virus itself in the first place. There have been many waves of COVID-19 and it only gets worse with each succeeding wave, hence, it is important to keep in mind that irrespective of whether there is a wave or not, we should continue to maintain social distancing, wear masks, sanitize our hands from time to time. Everyone should realize the seriousness of this pandemic and protect themselves and others.
Since, it is probable that this virus has several entry points to the brain and can cause depression or anxiety, clinicians can start early therapeutic treatment for patients who have been diagnosed with COVID-19 so that depression is less likely to affect the patient seriously. Early treatment can increase patients’ awareness about what is likely to happen next and so they have prepared themselves for it, and also reduce the solemnity of depression. Moreover, to further investigate the route of COVID-19 into the brain, researchers could find or develop a chemical that could be injected in COVID-19 patients such that when these patients go for MRI or any other radioactive diagnosis, the route of the virus can be seen. The chemical that would be injected would be responsible for following the path of the virus which can be viewed under radioactive radiations. Lastly, researchers could find more similarities between the structures of other viruses and COVID-19 and if there are similarities in the various parts of the viruses like proteins or their internal matter, then there is a chance that the mechanisms of COVID-19 to enter the brain are similar to those of other viruses.
References
Baig, A. (2020). Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host−Virus Interaction, and Proposed Neurotropic Mechanisms. ACS Chemical Neuroscience. Retrieved July 15, 2022, from https://pubs.acs.org/doi/pdf/10.1021/acschemneuro.0c00122
CDC. (2020, April 9). What is hepatitis C virus? CDC. Retrieved August 9, 2022, from https://www.cdc.gov/hepatitis/hcv/HepatitisCOverview.htm
Coughlin, S. (2012). Anxiety and Depression: Linkages with Viral Diseases. Anxiety and Depression: Linkages with Viral Diseases. Retrieved July 6, 2022, from https://link.springer.com/content/pdf/10.1007/BF03391675.pdf
Duarte, L. (2019, January 30). Herpes Simplex Virus Type 1 Infection of the Central Nervous System: Insights Into Proposed Interrelationships With Neurodegenerative Disorders. Frontiers. Retrieved August 11, 2022, from https://www.frontiersin.org/articles/10.3389/fncel.2019.00046/full
Government of Canada. (2021, May 31). Symptoms of anxiety and depression during the COVID-19 pandemic. Canada.ca. Retrieved August 9, 2022, from https://www.canada.ca/en/public-health/services/publications/diseases-conditions/sympto ms-anxiety-depression-covid-19-pandemic.html
Icke, D. (2017, January 11). Home. YouTube. Retrieved August 11, 2022, from https://www.bing.com/images/search?view=detailV2&ccid=3X2tisaO&id=7D576DB76 DF1AAC827B9EC7D66D5EBB1E5E41C64&thid=OIP.3X2tisaOdJ9RTw0un5yTBwHa FG&mediaurl=https%3A%2F%2Fthefreedomarticles.com%2Fwp-content%2Fuploads% 2F2020%2F07%2Fcribriform-plate-2.jpg&exph=55
Kim, E. (2021). Spike Proteins of SARS-CoV-2 Induce Pathological Changes in Molecular Delivery and Metabolic Function in the Brain Endothelial Cells. Spike Proteins of SARS-CoV-2 Induce Pathological Changes in Molecular Delivery and Metabolic Function in the Brain Endothelial Cells. Retrieved July 31, 2022, from https://www.mdpi.com/1999-4915/13/10/2021/htm
Liu, H. (2018). Mechanisms of Blood-Brain Barrier Disruption in Herpes Simplex Encephalitis. Mechanisms of Blood-Brain Barrier Disruption in Herpes Simplex Encephalitis. Retrieved July 15, 2022, from https://link.springer.com/article/10.1007/s11481-018-9821-6
Mayo Clinic. (2021, November 1). Influenza (flu) – Symptoms and causes. Mayo Clinic. Retrieved August 9, 2022, from https://www.mayoclinic.org/diseases-conditions/flu/symptoms-causes/syc-20351719
Mohammad, S. (2011). Influenza Virus Infection Aggravates Stroke Outcome. Influenza Virus Infection Aggravates Stroke Outcome. Retrieved July 12, 2022, from https://www.ahajournals.org/doi/full/10.1161/STROKEAHA.110.596783#d9655791e821 _copied
NASW. (2019). HIV/AIDS: General Overview. National Association of Social Workers. Retrieved August 1, 2022, from https://www.socialworkers.org/Practice/HIV-AIDs/HIV-AIDS-General-Overview
Natoli, S. (2020, May 22). Does SARS‐Cov‐2 invade the brain? Translational lessons from animal models. NCBI. Retrieved August 9, 2022, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7267377/
The New York Times. (2012, May 29). Adulthood: What the Brain Says About Maturity. The New York Times. Retrieved August 9, 2022, from https://www.nytimes.com/roomfordebate/2012/05/28/do-we-need-to-redefine-adulthood/ adulthood-what-the-brain-says-about-maturity
Stanculete, M. (2017, January 11). Home. YouTube. Retrieved August 11, 2022, from https://books.google.ca/books?hl=en&lr=&id=dHCQDwAAQBAJ&oi=fnd&pg=PA203 &dq=mechanism+of+hepatitis+C+virus+into+the+brain&ots=XzMPVFQCSb&sig=iJO9 RdculUoLKh0MFyhMuPIW8Mk&redir_esc=y#v=onepage&q=mechanism%20of%20 hepatitis%20C%20virus%20into%20the%20brain&f=fa
USC-News. (2017, January 11). Home. YouTube. Retrieved August 11, 2022, from https://www.bing.com/images/search?view=detailV2&ccid=NjkJeAdb&id=01522E0AB3 3B721D7FB6D455D69103E30094CA0D&thid=OIP.NjkJeAdb6YM-J59innAKFwHaHa &mediaurl=https%3A%2F%2Fpressroom.usc.edu%2Ffiles%2F2020%2F06%2Fundersta nding-coronavirus-022.jpg&exph=2251&expw=2
Weber, B. (2020, September 26). COVID-19 causing stress, depression and obsessive behaviour: survey. CTV News. Retrieved August 9, 2022, from https://www.ctvnews.ca/health/coronavirus/covid-19-causing-stress-depression-and-obses sive-behaviour-survey-1.5121426
WebMd. (2022, January 25). Symptoms of Coronavirus: Early Signs, Serious Symptoms and More. WebMD. Retrieved August 9, 2022, from https://www.webmd.com/lung/covid-19-symptoms#1
Wikipedia contributors. (2022). Angiotensin-converting enzyme 2. Wikipedia, The Free Encyclopedia. Retrieved August 7, 2022, from https://en.wikipedia.org/w/index.php?title=Special:CiteThisPage&page=Angiotensin-converting_enzyme_2&id=1096807192&wpFormIdentifier=titleform
Wikipedia contributors. (2022). COVID-19 pandemic. Wikipedia, The Free Encyclopedia. Retrieved August 10, 2022, from https://en.wikipedia.org/w/index.php?title=Special:CiteThisPage&page=COVID-19_pan demic&id=1102341524&wpFormIdentifier=titleform
Wikipedia Contributors. (2022). Olfactory nerve. Wikipedia, The Free Encyclopedia. Retrieved August 10, 2022, from https://en.wikipedia.org/w/index.php?title=Special:CiteThisPage&page=Olfactory_nerve &id=1080228277&wpFormIdentifier=titleform
Wikipedia Contributors. (2022). Olfactory nerve. Wikipedia. Retrieved August 11, 2022, from https://en.wikipedia.org/wiki/Olfactory_nerve
WLOX. (2017, January 11). Home. YouTube. Retrieved August 11, 2022, from
https://www.bing.com/images/search?view=detailV2&ccid=%2fjp1mfE8&id=E938B7FF 714F3025926A0EE153A9143AC37C4642&thid=OIP._jp1mfE8zrs0BzBRELIG-wHaEZ &mediaurl=https%3a%2f%2fwww.wlox.com%2fresizer%2fTCeRKcTY2uxZlbdP72x-0 m0WBUg%3d%2f1400x0%2fcloudfront-us-east-1.
Yeoh, S. (2018). Depression, fatigue and neurocognitive deficits in chronic hepatitis C. Depression, fatigue and neurocognitive deficits in chronic hepatitis C. Retrieved July 10, 2022, from https://link.springer.com/article/10.1007/s12072-018-9879-5
About the author

Sana Gupta
Sana is in her senior year of high school in Canada with a passion for Life Science. She takes keen interest in research opportunities to explore new dimensions in the medical field. Sana is also associated with many non-profit organizations and is the President of two clubs at her school. In her spare time, she enjoys dancing, listening to music, swimming, playing badminton, and making new friends.