
Author: Karishma Kulshrestha
Mentor: Dr. Andrew Franks
Thomas Worthington High School
Abstract
Migraine is the sixth most disabling illness in the world and the third most common (Saper, 2021). Many studies have found that migraines have numerous causes, which creates a wide variability in the effectiveness of treatments. In recent years, there has been exploration of alternative methods of treatment, such as music therapy. There have been many studies regarding music therapy and pain treatment, but very few specifically for headaches, and results have been inconclusive. The proposed research seeks to examine the extent to which predisposed beliefs about music therapy impact its efficacy when treating chronic migraines. Over the course of a six-week study, patients will be randomly assigned to one of two experimental treatment conditions whereby they will receive a combination or standard pharmaceutical treatment plus music therapy or standard pharmaceutical treatment plus therapeutic rhythmic class. Patients will also report the degree to which they perceive music therapy and other alternative treatments as effective pain-relieving measures. Patients will also report their pain symptoms weekly. It is anticipated that patients with stronger belief in the efficacy of music therapy, in particular, will experience greater reduction in pain symptoms when in the music therapy condition. The implications of an interaction between treatment efficacy beliefs and actual treatment effectiveness are discussed.
The Impact of Belief in Treatment Methodology on the Efficacy of Music Therapy in Those with Chronic Migraines
While many people have friends or family members who suffer from migraines, individuals who do not experience migraines themselves may be unaware of how chronic, unpredictable, and often mysterious migraine symptoms are. Approximately 1 billion people around the world have migraines (Pool, 2021), making migraines the third most prevalent illness in the world, along with being the 6th most disabling (Saper, 2021). Lipton et al. (2007) reported that 53.7% of those with migraines were severely impaired. Munakata et al. (2009) found that those with episodic migraine had direct and indirect costs of $1757 per year, and those with transformed migraine had costs of $7750 per year. Those who experience migraine–as well as their closest family and friends–are more likely to pursue knowledge regarding migraine causes and treatment (Saper, 2021), but they often find that migraines have many different causes and thus there is wide variability in types of treatment and their efficacy (Dodick & Gargus, 2008). Recently, there has been increasing interest in alternative treatments for migraine sufferers such as yoga (John et. al, 2007), risk factor modification (Schwedt, 2014), and music therapy (Diamante & Roxas, 2020). However, the degree to which such alternative treatments alleviate symptoms may be influenced by patients’ beliefs in their efficacy (e.g., Horne, 1999). Accordingly, the current research proposal seeks to examine how much predisposed beliefs about music therapy impact its efficacy, and if music therapy is actually effective in treating chronic migraines.
Music Therapy
Music therapy has been examined as a potential treatment for dementia (Vink et. al, 2003), generalized anxiety disorder (Gutiérrez & Camarena, 2015), as well as chronic migraine symptoms (Diamante & Roxas, 2020). Research on the use of music therapy as a treatment for migraines has demonstrated that it shows a significant improvement from no treatment (Oelkers-Ax, 2008). Music therapy has been shown to be effective for those seeking treatment for chronic migraine and tinnitus (Nickel et al., 2005). Additionally, Langenburg and colleagues (1995) did a case study on music therapy as treatment for someone with chronic migraines which demonstrated that it does lessen migraine symptoms. While additional studies have demonstrated similar efficacy for MT as a treatment for migraines (e.g., Diamante & Roxas, 2020), other studies have found that MT, while effective, is no more effective than other alternative treatments (Koenig, 2014). Moreover, music therapy can better improve executive functioning when it is able to provide functional support (Thaut & Hoemberg, 2017). Accordingly, we should expect music therapy to reduce migraine symptoms in patients when used in conjunction with standard treatment, but perhaps not more so than other distracting treatments. However, there are moderating factors that could influence the degree to which individual patients respond to alternative treatments such as music therapy–one of which may be their belief in the efficacy of music therapy.
Patient’s Beliefs in the Efficacy of Treatment
The ability of a patient’s belief in the efficacy of certain treatments to affect treatment outcomes has been examined in a variety of contexts. Patients’ beliefs about the type of treatment they’re receiving has been shown to impact the efficacy of that treatment (Horne, 1999). The symptoms of patients suffering from various illnesses were shown to respond more strongly to medical treatment among patients who believe more strongly in the effectiveness of traditional medicine as a treatment (Foulks et. al, 1986): the expectation of a drug’s impact on symptoms strongly influences the therapeutic efficacy of that drug (Bingel et al, 2011). Similarly, Clatworthy et. al found that patients better adhered to their treatment plan when they believed that it would work, and thus they found more benefits from their treatment (2007). In addition, a study regarding the effects of methotrexate on rheumatoid arthritis symptoms found similar results (de Thurah et. al, 2009). Studies have also demonstrated that beliefs regarding severity of the patient’s illness impact the efficacy of the treatment (Marks et al., 1986). However, to the best of our knowledge, no research has yet investigated this moderating influence regarding the efficacy of music therapy in migraine treatment. Accordingly, the current research will assign patients to two conditions of music therapy, one who has strong beliefs in the efficacy of music therapy, and one who does not. These two groups will demonstrate the relationship between belief in the efficacy of treatment and pain reduction.
Research Hypothesis: We expect that the efficacy of music therapy, in comparison to a different alternative treatment, in reducing migraine symptoms will be moderated by patients’ beliefs in music therapy’s effectiveness. Specifically, we expect that the relative efficacy of music therapy, in comparison to yoga therapy, in relieving chronic pain symptoms will be greater among individuals who already perceive music therapy as an effective treatment.
Method
Participants
Participants will be recruited from a hospital circuit, through compliant doctors asking their patients with chronic migraines. They will be given a small monetary sum, and the study will be conducted in an academic center with music facilities.
Measures
Belief in Treatment Efficacy. Prior to being randomly assigned to a treatment condition, patients will fill out a brief survey asking them to report how effective they believe each of the following therapies would be for reducing their migraine symptoms: music therapy, rhythmic class, yoga, mindfulness meditation, traditional western medicine, and pet therapy (Appendix A). Brief descriptions of each therapy type will accompany the items. Participants will indicate their belief in the efficacy of each therapy on a 1 (“Not at All Effective”) to 7 (“Highly Effective”) Likert-type scale. The variable of interest is patients’ beliefs in the efficacy of music therapy, and patients will be told that their beliefs will not affect the treatment condition to which they are assigned.
Treatment Condition. Patients will be randomly assigned to receive one of two treatments in addition to traditional pharmaceutical treatment: music therapy or rhythmic class This treatment manipulation is similar to one used in previous research (Gutgsell et. al 2013). In each condition, patients will undergo their additional treatment 3 times per week. Patients in the music therapy condition will go into a dark room without distractions for 20 minutes and have a music therapist play harp pieces for them. Patients in the rhythmic class (Bozorg-Nejad et. al 2018) condition will go into a dark room without distractions for 20 minutes and will be taught how to control the various paces of the body with breathing. These conditions will last for 6 weeks.
Improvement of Symptoms. The dependent variable that will be measured is the difference in pain before treatment and after treatment using a standardized scale. Patients will rate their overall severity of their symptoms at the end of each week on a scale from 0 (“No Symptoms”) to 10 (“Emergency Treatment Necessary”) similar to measures of migraine pain used in previous research (Jensen et. al 1999). Average scores from the final three weeks will be subtracted from average scores from the first three weeks to determine the change in symptoms over the treatment period.
Procedure
When first agreeing to participate in the study, the participants will complete an informed consent document. They will be given their monetary reimbursement of $50 for their time, and then will be separated into two groups, after being sent and completing the survey about their beliefs in the efficacy of music therapy remotely. From those two groups they will be randomly assigned to either the music therapy condition or the rhythmic class, depending on what time of day they fill out the survey. They will then go to these therapies at least three times per week for 20 minutes for six weeks. Over the course of these six weeks their pain symptoms will be monitored and recorded through their respective nurses on the standardized scale in Appendix B.
Results
Correlational Analyses
A zero-order Pearson correlational analysis will be conducted to assess the relationship between belief in the efficacy of music therapy and improvement of pain symptoms for patients in the MT condition only. We hypothesize that, among patients in the MT condition, higher belief in MT will predict more improvement of symptoms. We expect to see a similar correlation between belief in the effectiveness of rhythmic class in the comparison condition.
T-Test
A t-test will be conducted to compare symptom improvement between the two experimental groups. We expect that without taking into account the patients’ beliefs in MT’s effectiveness that patients in the MT conditional will not show significantly more or less improvement than patients in the rhythmic class condition.
Moderation Analysis
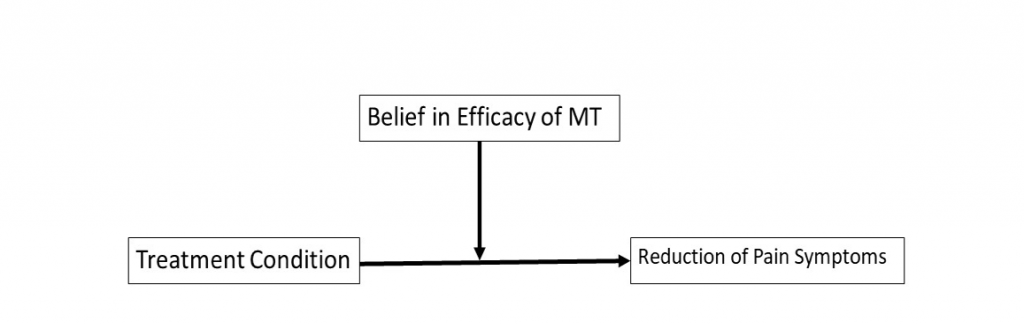
To test our primary research hypothesis, a moderation analysis will be conducted using the PROCESS macro (Hayes, 2013) Model 1. Treatment condition will be added to the model as the independent variable (x), belief in the efficacy of music therapy as the moderator (w), and symptom improvement as the dependent variable (y). We predict that belief in the efficacy of MT will moderate the difference between treatment groups such that MT will be more effective than rhythmic class among participants with higher beliefs in MT’s efficacy. The conceptual model is illustrated in Figure 1.
Discussion
The proposed study seeks to explore the relationship between patients’ beliefs in the efficacy of alternative forms of treatment for chronic pain and the actual effectiveness of those treatments. In particular, this study intends to focus on music therapy (MT) as a potential treatment. Patients’ beliefs about MT, and other alternative treatments, will be measured prior to random assignment to a treatment condition that includes typical pharmaceutical treatment plus either music therapy or a comparison treatments condition. It is hypothesized that beliefs in the efficacy of MT will interact with assignment to the MT condition such that patients who perceive MT as more effective and are assigned to the MT condition will experience more pain symptom relief over the course of the study.
Implications
Approximately 5-12% percent of people worldwide suffer from migraines (MacGregor et. al, 2003), which is millions of people. Therefore, the majority of people at least know someone who is a victim of this kind of pain. Additionally, making strides within the treatment of these migraines could vastly improve quality of life. Music therapy specifically is an instance of alternative methods, based on other facts. If the experimental hypothesis was supported, then pain treatment would be reimagined to adjust to the beliefs of the patient. To ensure the best outcomes, physicians could prescribe whichever alternative treatment an individual patient has the most positive views of in addition to pharmaceutical treatment. Additionally, results that support our hypotheses would suggest that physicians should emphasize scientific support for alternative methods to their patients. Doing so may make beliefs about such treatments more positive, which would in turn make the treatments more effective.
Limitations
This study would be done on adults, so it probably would not be as conclusive for the same study done on children or adolescents. The proposed study also does not account for potential disparities among those who have chronic migraines. This study also would not discuss the musical aspect involved in rhythm. The proposed study also does not account for the influence of those providing the treatment on the patient’s belief in efficacy. This study also only compares two types of alternative therapies, when there are many others which could have different results.
Future Directions
In future studies, there should be much deliberation regarding the control therapy and how it relates to music therapy. There could be focus on how different types of music impact the efficacy, or how it relates to what is being treated. . For instance, it has been shown that music can help those with dementia express themselves with language (Brotons & Kroger, 2000). Moreover, connecting these two things is something worth looking into, based on how music has a unique impact on the brain and has helped lessen the impacts of other neurological disorders. As far as pain management goes, it is important to consider the different ways that people can feel pain and how each experience it unique, along with the wide variety of treatment methods- beyond the ones discussed in this proposal.
References
Bingel, U., Wanigasekera, V., Wiech, K., Mhuircheartaigh, R. N., Lee, M. C., Ploner, M., & Tracey, I. (2011). The effect of treatment expectation on drug efficacy: imaging the analgesic benefit of the opioid remifentanil. Science translational medicine, 3(70), 70ra14-70ra14.
Bozorg-Nejad, M., Azizkhani, H., Ardebili, F. M., Mousavi, S. K., Manafi, F., & Hosseini, A. F. (2018). The effect of rhythmic breathing on pain of dressing change in patients with burns referred to ayatollah mousavi hospital. World journal of plastic surgery, 7(1), 51.
Brotons, M., PhD, MT-BC, Koger, S. PhD, The Impact of Music Therapy on Language Functioning in Dementia, Journal of Music Therapy, Volume 37, Issue 3, Fall 2000, Pages 183–195, https://doi.org/10.1093/jmt/37.3.183
Clatworthy, J., Bowskill, R., Rank, T., Parham, R., & Horne, R. (2007). Adherence to medication in bipolar disorder: a qualitative study exploring the role of patients’ beliefs about the condition and its treatment. Bipolar disorders, 9(6), 656-664.
de Thurah, A., Nørgaard, M., Harder, I. et al. Compliance with methotrexate treatment in patients with rheumatoid arthritis: influence of patients’ beliefs about the medicine. A prospective cohort study. Rheumatol Int 30, 1441–1448 (2010). https://doi.org/10.1007/s00296-009-1160-8
Foulks, E. F., Persons, J. B., & Merkel, R. L. (1986). The effect of patients’ beliefs about their illnesses on compliance in psychotherapy. The American Journal of Psychiatry, 143(3), 340–344. https://doi.org/10.1176/ajp.143.3.340
Gutiérrez, E. O. F., & Camarena, V. A. T. (2015). Music therapy in generalized anxiety disorder. The Arts in Psychotherapy, 44, 19-24.
Gutgsell, K. J., Schluchter, M., Margevicius, S., DeGolia, P. A., McLaughlin, B., Harris, M., … & Wiencek, C. (2013). Music therapy reduces pain in palliative care patients: a randomized controlled trial. Journal of pain and symptom management, 45(5), 822-831.
Horne, R. (1999). Patients’ beliefs about treatment: The hidden determinant of treatment outcome?[Editorial]. Journal of Psychosomatic Research, 47(6), 491–495. https://doi.org/10.1016/S0022-3999(99)00058-6
Jensen, M. P., Turner, J. A., Romano, J. M., & Fisher, L. D. (1999). Comparative reliability and validity of chronic pain intensity measures. Pain, 83(2), 157-162.
John, P., Sharma, N., Sharma, C.M. and Kankane, A. (2007), Effectiveness of Yoga Therapy in the Treatment of Migraine Without Aura: A Randomized Controlled Trial. Headache: The Journal of Head and Face Pain, 47: 654-661
Koenig J. Music therapy in the treatment of primary headache disorders. OA Alternative Medicine 2014 Jan 18;2(1):1
Langenberg, M., Frommer, J., & Tress, W. (1995). Music therapy single case research–a qualitative approach. Psychotherapie, Psychosomatik, medizinische Psychologie, 45(12), 418-426.
MacGregor, E. A., Brandes, J., & Eikermann, A. (2003). Migraine prevalence and treatment patterns: the global Migraine and Zolmitriptan Evaluation survey. Headache: The Journal of Head and Face Pain, 43(1), 19-26.
Lipton, R. B., Bigal, M. E., Diamond, M., Freitag, F., Reed, M. L., & Stewart, W. F. (2007). Migraine prevalence, disease burden, and the need for preventive therapy. Neurology, 68(5), 343-349.
Marks, G., Richardson, J. L., Graham, J. W., & Levine, A. (1986). Role of health locus of control beliefs and expectations of treatment efficacy in adjustment to cancer. Journal of personality and social psychology, 51(2), 443.
Munakata, J., Hazard, E., Serrano, D., Klingman, D., Rupnow, M. F., Tierce, J., … & Lipton, R. B. (2009). Economic burden of transformed migraine: results from the American Migraine Prevalence and Prevention (AMPP) Study. Headache: The Journal of Head and Face Pain, 49(4), 498-508.
Oelkers-Ax, R., Leins, A., Parzer, P., Hillecke, T., Bolay, H. V., Fischer, J., … & Resch, F. (2008). Butterbur root extract and music therapy in the prevention of childhood migraine: an explorative study. European Journal of Pain, 12(3), 301-313.
Thaut, M. H. (2010). Neurologic music therapy in cognitive rehabilitation. Music Perception, 27(4), 281-285.
Vink, A. C., Bruinsma, M. S., & Scholten, R. J. (2003). Music therapy for people with dementia. Cochrane database of systematic reviews, (4).
Appendix A
Questionnaire for measuring belief in efficacy of music therapy.
How confident are you in the ability of pet therapy to treat your pain?
1 2 3 4 5 6 7
Not at all Extremely
confident confident
How confident are you in the ability of rhythmic classes to treat your pain?
1 2 3 4 5 6 7
Not at all Extremely
confident confident
How confident are you in the ability of yoga to treat your pain?
1 2 3 4 5 6 7
Not at all Extremely
confident confident
How confident are you in the ability of music therapy to treat your pain?
1 2 3 4 5 6 7
Not at all Extremely
confident confident
How confident are you in the ability of traditional western medicine to treat your pain?
1 2 3 4 5 6 7
Not at all Extremely
confident confident
How confident are you in the ability of mindfulness meditation to treat your pain?
1 2 3 4 5 6 7
Not at all Extremely
confident confident
Appendix B
Measurement of pain
How would you rate your pain symptoms this week??
1 2 3 4 5 6 7 8 9 10
No symptoms
About the author

Karishma Kulshrestha
Karishma is currently a Senior at the Thomas Worthington High School in Ohio. She has a strong passion for people, and her extraverted nature is where this seed was planted. As someone with chronic migraines herself, she has seen a lot of the medical systems from the patient perspective which has allowed her to think about things others might not normally. Karishma is in marching band and was a drum major this year. She also plays volleyball, and started a ski club at her school.
