Author: Rishya Gutti
Neuqua Valley High School
Introduction
Patellofemoral injuries occur when the structures that join the kneecap with the femur are injured, stressed, or torn. Many times, these injuries stem from underlying patellar instability which then contributes to symptoms including but not restricted to anterior knee pain and patellar subluxation/dislocation. It is important to understand that this type of injury is seen with specific mechanisms of injury, many of which involve a jumping motion and the subsequent landing or repeated stress, such as running. This review will not only delve into the anatomy and etiology of patellofemoral pain syndrome (PFPS), but also discuss the treatment and rehabilitation associated with it as well.
Pathology/Anatomy:
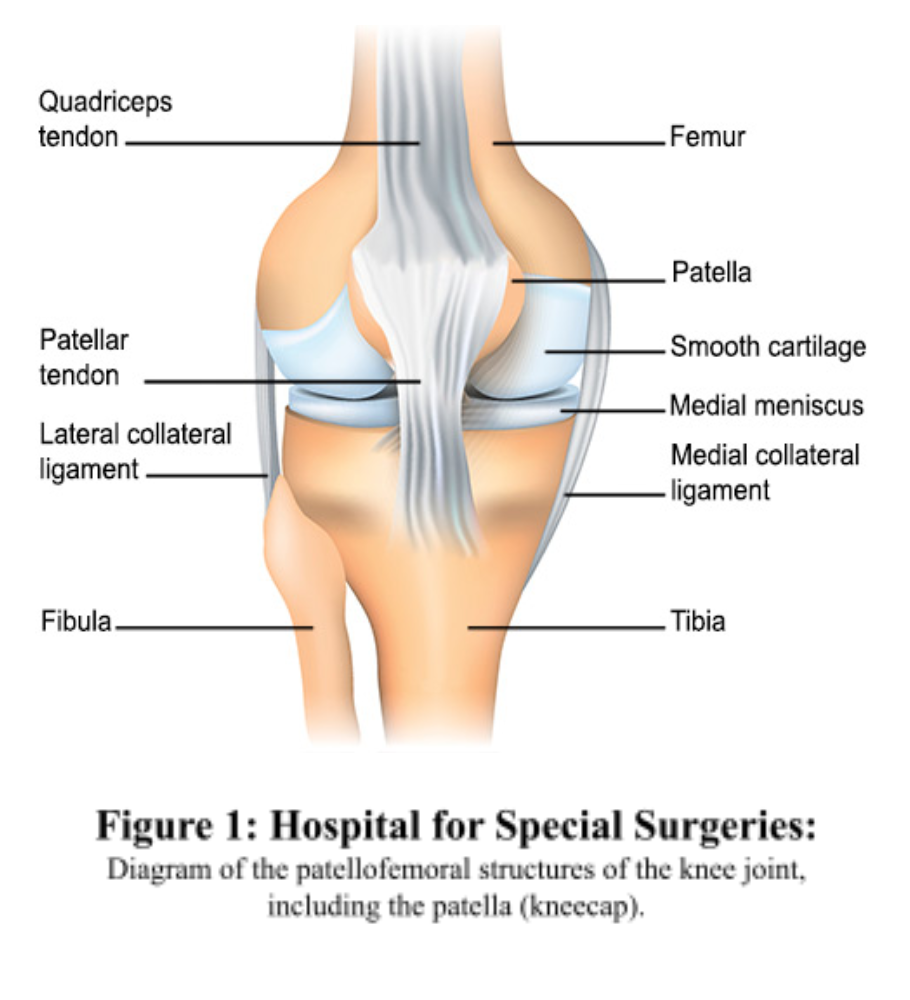
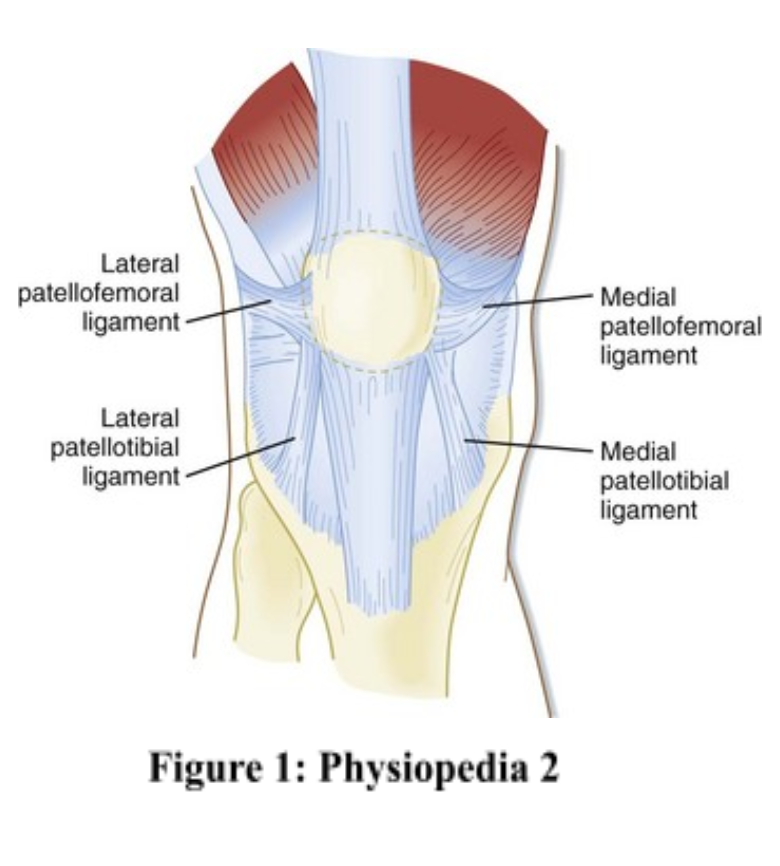
Overall, patellofemoral pain syndrome is an overarching term regarding pain in any of the structures that compose the joint and the surrounding tissues and ligaments (Physiopedia 1). This joint consists of the bony structures of the patella and the femur, along with, mainly, the lateral and medial collateral ligaments (LCL/MCL) and the lesser known epi condylopatellar, menisco patellar, medial patellofemoral, and lateral patellofemoral ligaments.
Additionally, there are also many bursae that are within this region in order to cushion the impact the knee experiences (Physiopedia 1). The patella is the largest sesamoid bone in the human body, and is roughly shaped like an upside down triangle. It has 2 main facets in the back and a vertical ridge in between that divides the two. These two facets line up with the condyles of the femur, and the lateral condyle is deeper than the medial in order to compensate for the more severe stress and pull on this side than the other (Physiopedia 2). Along with the bony structures, the ligaments are the other part of the static system in this joint. The MCL and LCL are important stabilizers of this joint and both originate from the femur. However, the MCL inserts at the tibial head, whereas the LCL inserts at the fibular head. These ligaments counteract lateral stresses on the knee, but are also subject to rupture if they are subject to excessive valgus or varus force. In addition to these structures, The Medial Patellofemoral Ligament (MPFL) and the Lateral Patellofemoral Ligament (LPFL) also contribute to the stability of the patellar bone itself. Each originate at their respective femoral condyles and insert at the medial and lateral sides of the patella. The MPFL provides a medial force to keep the patella tracking the correct direction, and the LPFL does the same on its side (Physiopedia 2). If these ligaments are torn, lateral or medial subluxation or dislocation may be experienced. Lastly, the largest and strongest muscle of the joint is the quadriceps. This muscle extends the joint and is made of the rectus femoris and the vastus group. The vastus group is made of the vastus lateralis and the vastus oblique. The vastus lateralis helps with patellar tracking and the vastus oblique stabilizes the patella against lateral force.
Etiology/Mechanism
With Patellofemoral Injury being a blanket term, there are numerous causes and injuries that may stem from this. One cause of patellofemoral pain is the orientation of the bone itself that induces improper tracking which then leads to instability (Physiopedia 1). Moreover, if there is an imbalance in muscular strength, this can also contribute to the pain as one side is being pulled more than the other. Another cause of the syndrome is flat feet which can cause the knee to fall inwards. The lack of foot arch leads to the foot falling flat which then causes the knee to also follow suit and become valgus rather than its normal line up (Han,Y. et.al. 2017). Some common stresses that also contribute to this variety of injury are running, jumping, and other repeated impact-type stresses (Shubin Stein et.al. 2016, Oct.). Additionally, patellofemoral pain syndrome is more seen in women rather than men. This is due to women standing and squatting in more valgus positions than men and this contributes to uneven stress distribution (Shubin Stein et.al. 2016, Oct.).
Signs and Symptoms
Many times, the signs and symptoms are the cause of the problem itself; for example, a symptom such as flat feet could be a sign of patellofemoral pain, but it is also a cause of it. Some symptoms that follow a similar pattern are weak quadriceps (or portion of the quads), tight iliotibial band, tight hamstrings, weak or tight hip muscles, and tight calf muscles (Physiopedia 1). All of these cause an imbalance in how the knee is pulled, which then contributes to the pain that follows. Moreover, certain activities may aggravate the pain, such as running, jumping, and squatting. The patient may also present with pain when going up and down stairs, bending their knees, and lunging; popping or crackling noises may be heard when standing up from a sitting position or when ascending stairs (Mulcahey et.al. 2020).
Treatment
NON-SURGICAL:
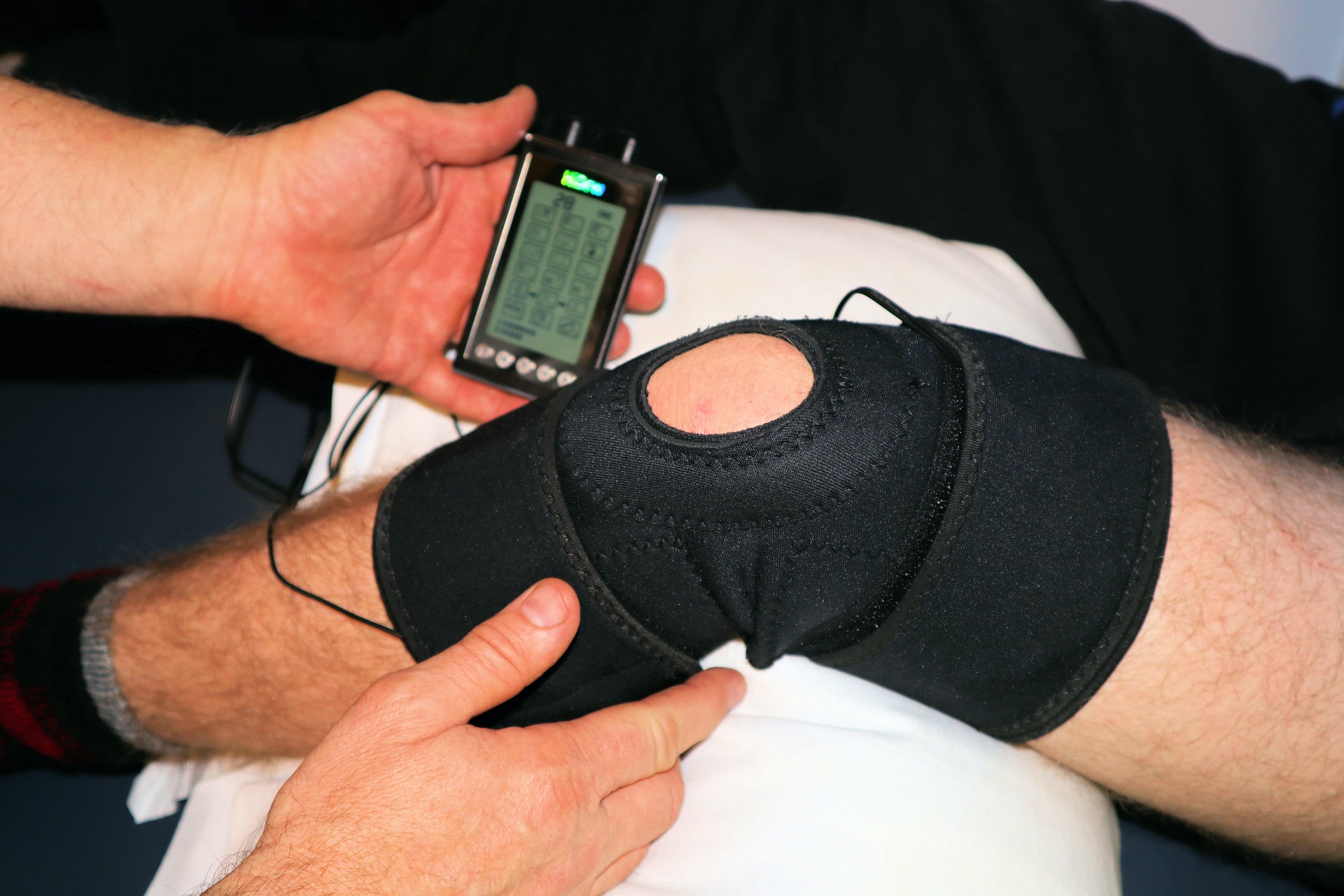
Simple changes, such as activity substitution could help with relieving the pain, and avoiding activities that are known to aggravate the injury can also work, depending on the severity of the pain. Low impact activities, such as riding a bike or swimming could substitute high impact ones. The RICE method (rest, ice, elevation, compression) can also assist in relieving pain as it will bring down inflammation to the joint. Anti-inflammatory medications, such as NSAIDs can also be taken to remediate symptoms (Mulcahey et.al. 2020). Additionally, physical therapy can be done to strengthen the surrounding structures of the knee, improve range of motion, and build endurance. Lastly, orthotics can be worn in shoes to help with flat feet and provide an arch to the foot so that the knee does not fall into valgus. These can be purchased at a store or online, or they can be custom made to fit what the patient specifically needs (Mulcahey et.al. 2020).
SURGICAL:
Surgical treatments are used conservatively, and only in instances when it is absolutely needed. Most of the surgical options are performed arthroscopically, where small incisions are made as needed and small tools, along with the assistance of a camera, are used rather than opening up the whole knee. This results in less scarring in the future after healing. Some instances where surgical intervention is needed is for cartilage debridement or if the patient has experienced multiple subluxations or dislocation of the patella, in which case a MPFL reconstruction may be needed (Shubin Stein et.al. 2016, June).
Rehabilitation
Rehab for this injury mostly consists of quadriceps strengthening and stretching, along with surrounding muscles. Some stretches that are commonly implemented include calf wall stretch, standing quad stretch, and lying hamstring wall stretch (Healthwise Staff). Some strengthening exercises done include, but are not limited to quad sets, where the affected knee is placed on a rolled towel and quads are tightened by pushing the knee into the towel, lying straight leg raises to the front and back, and wall assisted squats (Healthwise Staff). Rehab for these injuries can take anywhere from 4-7 months if it is surgical, but much of the time, these rehab exercises need to be completed consistently over an indefinite period of time, especially if the injury is non-surgical. Ultimately, the exercises will help remediate the imbalance and can help with pain.
Prevention
The prevention of patellofemoral pain syndrome is essentially the goal of the rehab program for it. Strengthening the quadriceps and making sure that any imbalances are taken care of is extremely important in this case. Wearing the right shoes, doing low impact exercises, cross training to take the load off the knee, and being aware of what causes symptoms and what does not is also extremely important. Studies have also shown that certain taping techniques, when used in conjunction with strengthening exercises, can assist in pain relief and recovery from PFPS (Logan et.a. 2017).
Conclusion
Over the course of this review, patellofemoral pain syndrome was discussed in great detail. Throughout this joint, there are many structures that comprise it, mainly the patellar bone, the femur, and various ligaments and muscle groups. PFPS can be the result of any one of these structures being injured, but the method of injury is quite common between them. Oftentimes, it is high impact activities that instigate the pain, and this syndrome is seen more in women than men. There are many ways of treatment, rehabilitation, and prevention of injury, all ranging from basic strength work to surgery. Overall, to maintain a healthy patellofemoral joint, it is important to gauge activity, be aware of what causes pain, and be proactive in how that pain is managed or treated.
References
Kujala, U M et al. “Scoring of patellofemoral disorders.” Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association vol. 9,2 (1993): 159-63. doi:10.1016/s0749-8063(05)80366-4
(1) Patellofemoral Pain Syndrome. (2022, February 28). Physiopedia, . Retrieved 13:48, May 13, 2022 from https://www.physio-pedia.com/index.php?title=Patellofemoral_Pain_Syndrome&oldid=295866.
Loudon J. K. (2016). BIOMECHANICS AND PATHOMECHANICS OF THE PATELLOFEMORAL JOINT. International journal of sports physical therapy, 11(6), 820–830.
(2) Patellofemoral Joint. (2022, February 28). Physiopedia, . Retrieved 16:46, May 14, 2022 from https://www.physio-pedia.com/index.php?title=Patellofemoral_Joint&oldid=295861.
Shubin Stein, B. E., & Strickland, S. M. (2016, October 26). Patellofemoral Disorders: An Overview. Hospital for Special Surgery. Retrieved May 14, 2022, from https://www.hss.edu/conditions_patellofemoral-disorders-overview.asp
Han, Y., Duan, D., Zhao, K., Wang, X., Ouyang, L., & Liu, G. (2017). Investigation of the Relationship Between Flatfoot and Patellar Subluxation in Adolescents. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons, 56(1), 15–18.
Mulcahey, M. M., Hettrich, C. M., & Liechti, D. (2020, October). Patellofemoral Pain Syndrome.OrthoInfo. Retrieved May 14, 2022, from https://orthoinfo.aaos.org/en/diseases–conditions/patellofemoral-pain-syndrome/
Shubin Stein, B. E., & Strickland, S. M. (2016, June 27). Medial Patellofemoral Ligament (MPFL) Reconstruction. Hospital for Special Surgery. Retrieved May 14, 2022, from https://www.hss.edu/conditions_medial-patellofemoral-ligament-reconstruction-mpfl.asp
Healthwise Staff. (2021, July 1). Patellofemoral Pain Syndrome (Runner’s Knee): Exercises. Alberta Healthcare. Retrieved May 14, 2022, from https://myhealth.alberta.ca/Health/aftercareinformation/pages/conditions.aspx?hwid=bo1601
Logan, C. A., Bhashyam, A. R., Tisosky, A. J., Haber, D. B., Jorgensen, A., Roy, A., & Provencher, M. T. (2017). Systematic Review of the Effect of Taping Techniques on Patellofemoral Pain Syndrome. Sports health, 9(5), 456–461. https://doi.org/10.1177/1941738117710938
Diagram of the patellofemroal structures of the knee joint, including the patella (kneecap). [Image]. (n.d.). Hospital for Special Surgery. https://www.hss.edu/ condition-list_patellofemoral-disorders.asp
About the author

Rishya Gutti
Rishya is currently a junior at Neuqua Valley High School. She interested in the biological sciences and is an aspiring medical student. Research programs like RISE (Research, Inquiry Skills & Experimentation) have equipped Rishya with the necessary skills to conduct independent research. She is a third degree black belt in Taekwondo and has won several national titles in her age group. Rishya enjoys volunteering her time to teach mathematics to younger students and to promote mental health awareness through a non-profit organization. In her free time, you will find her reading, working out or watching her favorite tv shows.